The CX 2020 LIVE Vascular Access Consensus session sparked global interest, with chair Nick Inston (Birmingham, UK) and moderator Domenico Valenti (London, UK) taking questions from 17 countries, spanning South America to South East Asia. The session pinpointed the latest developments in this fast-moving field, including cutting-edge technologies, such as endovascular arteriovenous fistula (endoAVF) creation, the use of covered stents in dialysis access, and the advantages of external support. Jennifer Hanko (Belfast, UK) opened with the benefits and drawbacks of peritoneal dialysis compared to haemodialysis, stressing the importance of choosing “the right access, for the right patient, at the right time”. Polling revealed that audience members were split on whether endovascular fistula creation is the future, with Inston concluding that the topic is “still up for debate”.
“All modalities must be considered” when planning access, Hanko began, including peritoneal access, haemodialysis, conservative care “as appropriate,” and the patient’s suitability for kidney transplantation.
 She suggested that more patients could benefit from peritoneal dialysis if they had it first, but also stressed that this approach is only recommended for certain patients. Indeed, while haemodialysis requires frequent hospitalisation and peritoneal dialysis can be managed at home, the latter does carry with it a risk of infection.
She suggested that more patients could benefit from peritoneal dialysis if they had it first, but also stressed that this approach is only recommended for certain patients. Indeed, while haemodialysis requires frequent hospitalisation and peritoneal dialysis can be managed at home, the latter does carry with it a risk of infection.
Among the factors that preclude peritoneal dialysis are the presence of cardiovascular disease, low serum albumin, and age greater than 75 years. Furthermore, Hanko noted that there is “no consensus” on when a patient should proceed to both peritoneal dialysis catheter and back-up fistula creation.
Patients with no fistula options “should be encouraged to do peritoneal dialysis if possible,” Hanko advised the CX 2020 LIVE audience.
“Traditionally, we have advocated radiocephalic fistula first.” However, Hanko acknowledged that there are situations in which this may not be appropriate. She pointed out that patient choice is also an important factor, summarising that the approach at the Belfast City Hospital “is no longer fistula first. It is the right access, for the right patient, at the right time”.
Valenti opened the discussion after Hanko’s presentation, asking how patient choice influences her decision-making in fistula creation. “I think it is a partnership,” Hanko replied, adding that “it is about working with [patients] to get to a solution”.
Inston asked whether it is common practice to insert a peritoneal dialysis tube at the same time as creating a fistula, to which Hanko responded that it is not something she would advocate for most patients. But she acknowledged that a “small subset, probably less than 5%” would benefit. “I think we can all testify to the fact that when patients fail peritoneal dialysis, we are not always that great at having their vascular access ready”.
In response to a question from the UK, about what to do if fistula formation is not what the patient wishes, Hanko said she would still strongly recommend it, and get additional education for the patient on the risks versus benefits of a catheter over a fistula. However, she noted that “it is the patient’s choice in the end”.
New era of vascular access must move beyond “fistula first” approach

David Kingsmore (Glasgow, United Kingdom) also advocated a patient-tailored outlook to vascular access, describing in his presentation the “old era” approach of “fistula provision for all”—typified, he said, by European Society for Vascular Surgery (ESVS) 2018 guidelines on vascular access—as being ripe for change, in particular through greater use of early cannulation arteriovenous grafts (ecAVGs).
Kingsmore made the point that while, for some patients, fistulas remain the ideal treatment option, “for half [of patients] they are not”. Likewise, catheters for some patients are ideal, he commented, but for most they are not. “You have to consider what the patient aim is, and how to incorporate transplant with our vascular access planning. Overall, early cannulation grafts are certainly under-utilised and they can be optimised. We have an opportunity for a new era, to integrate and tailor optimal practices to patients’ aims, choices, and needs.”
Following his presentation, Valenti asked Kingsmore whether the “fistula first” approach has contributed to the underutilisation of grafts, to which he replied: “We are victims of looking at procedures rather than patients, [and] not integrating with other services and patient outcomes. Nick [Inston] has talked before about the outcomes and the changing success rate. We have got to bear in mind that dialysis has evolved substantially over the years, and transplant has evolved even more.”
Support for the use of external reinforcement is still limited

Developments in the use of external support devices were outlined by Robert Shahverdyan (Hamburg, Germany), who put forward a mechanical solution for fistula failure.
And, although an online poll of participants found that only 17% are currently using these devices to improve fistula outcomes, Inston was confident that the numbers would grow following Shahverdyan’s presentation on VasQ (Laminate Medical).
“The VasQ device improves the likelihood of an AVF becoming functional by addressing both haemodynamic and mechanical factors of failure. It produces consistent clinical benefits to patients, and also improves outcomes for an individual clinic when adopted as the standard of care for AVF creation.
“Several studies have been performed and more are under way to validate the clinical benefits of VasQ. So far, we are observing consistently high AVF usability and patency outcomes across the studies: 80–90% usability, with roughly 80% primary patency at six months for VasQ. [This] compares favourably with most other published results for standard AVF creations.”
Experience with endoAVF “encouraging,” but more data needed
Robert Jones (Birmingham, UK) provided a technology update on endoAVF, looking at the performance of two catheter systems—Ellipsys (Avenu Medical) and WavelinQ (BD).
One of the major benefits with this approach is the lack of surgical trauma, “therefore potentially less intimal hyperplasia and stenosis formation”. Jones also highlighted: “Both of these catheter systems utilise the forearm vascular anatomy to create an endoAVF, an area that is not typically used for surgical fistula creation”.
He added: “Multiple specialty operators can use both devices to create successful fistulas and this potentially can lead to a decreased waiting time for definitive access. Of utmost importance is patient preference.”
Polling reveals audience split over whether endovascular fistula creation is the way forward
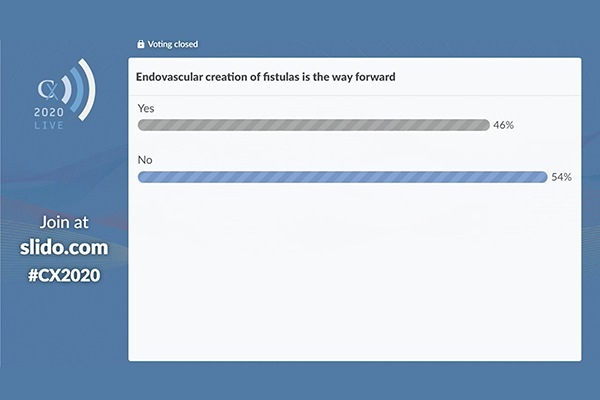
Polling of the online audience revealed that only 46% agreed with the statement: “Endovascular creation of a fistula is the way forward.” However, if a role for durability of the fistula can be established, consensus may be reached. In the discussion that followed the presentation, a participant from Buenos Aires in Argentina raised the issue of the difference in cost between endoAVF formation and a standard surgical procedure. Jones conceded that “the upfront cost of an endoAVF device is higher in most countries than it is for surgical fistula”. But he pointed out: “The evidence to date has demonstrated that these endoAVFs require less reinterventions.” Jones pointed to the potential for longer-term savings, citing an American study published in the Journal of Vascular Access that compared collective WavelinQ data with retrospective Medicare data that “demonstrated that there was a saving to be made in each patient over a period of time. The upfront costs are certainly more expensive with these devices but, overall, in a long period of time, according to the evidence, it suggests there is a cost saving.”
Edited case illustrates endovascular fistula creation with WavelinQ
Panagiotis M Kitrou (Patras, Greece) demonstrated an edited case on the endovascular creation of an arteriovenous fistula using WavelinQ.
The device consists of two rapid change catheters, with the arterial catheter inserted first. Kitrou detailed the steps involved in preparing the patient, as well as the other devices required for the procedure.
The issue of costs associated with endoAVF was raised again in the discussion that followed, with a question from Johannesburg in South Africa. Other queries on time-to-fistula maturation in endoAVF, and whether it is necessary to coil deep veins, were submitted from as far afield as Argentina and Pakistan.
Covered endoprostheses are “the gold standard” for venous anastomosis with prosthetic vascular access
A second edited case was presented by Matteo Tozzi (Varese, Italy) on the use of a self-expanding covered endoprosthesis—Viabahn (Gore)—to treat AVF failure at the venous anastomosis. Tozzi reviewed the case of a 69-year-old male receiving haemodialysis for diabetic nephropathy, starting the dialysis with a tunnelled central venous catheter filter for a bloodstream infection.
Following the edited case, Tozzi then fielded questions from the global audience, including one from India to which Tozzi responded by outlining that “in the cephalic arch, the stent graft is the first option for the stenosis because all other techniques such as drug-coated balloon, plain balloon or high-pressure balloon fail very fast”. In this instance, a covered stent graft is “the gold standard”.
Tozzi added that he “chose this terrible case to demonstrate the ability to maintain patency in the functionality of the early cannulation graft” and following a question from a physician in Malaysia, about the use of cutting or scoring balloons before deploying the stent graft, Tozzi noted that “I prefer scoring balloons for predilatation of arch stenosis like the prosthetic venous anastomosis. I do not use cutting [balloons] because the blade damages the elasticity of the internal lamina of the vessel and therefore increases the intimal hyperplasia.”