Nikos Giannikas and Panos Kitrou (Patras, Greece) write together about the role that endothelial tight junctions play in vascular access, evidence from previous studies, and a proposed upcoming study that aims to evaluate the expression of the main tight junctions (TJ) proteins at the endothelium of end-stage kidney disease (ESKD) patients.
Stenosis is the Achilles’ heel of vascular access, leading to dysfunction and compromised haemodialysis. Owed to several factors, the histopathologic entity responsible for this is described as venous neointimal hyperplasia (VNIH).1 The latter is mainly attributed to vascular injury, inflammation and haemodynamic stress which triggers contractile smooth muscle cells and myofibroblast proliferation migrating to the area of stenosis. These cells produce extracellular matrix which, together, create an aggressive fibromasular thickening.2,3
Chaudhury et al stated that high levels of urea exacerbate the endothelial dysfunction, possibly through pathways of inflammation and oxidative stress. Moreover, urea was held responsible for the development of neointimal hyperplasia in both chronic-kidney disease (CKD) and ESKD patients without previous vascular access placement.1,4
Vazari et al described in their article how, in an animal experimental study, pathologic urea levels—along with other retained toxins—exert a change in the microbiome of the gut, while the presence of uraemia alone provokes disruption of the intestinal epithelium, a pathological entity known as “leaky gut”.5 Their study showed the impact of uraemia in the paracellular pathway of the epithelium. According to the authors, urea highly affects the main constituent of the paracellular pathway, the TJ, which act as the blood-gut barrier. Blood-gut barrier malfunction (even at the early stage of the CKD) allows a plethora of toxins to enter the systematic circulation and further deteriorate the kidney function. A recent single-centre, non-randomised clinical study involving 44 patients—divided into three groups—demonstrated that ESKD patients had significantly reduced intestinal levels of occludin and claudin, as confirmed by duodenal biopsies. These reductions were correlated with systemic endotoxemia when compared to the control group.6 Thus, once the intestinal barrier is disrupted in CKD, the translocation of bacteria-derived uremic toxins and other noxious luminal contents into the systemic circulation induce inflammation, vascular calcification, insulin resistance, decreased bone turnover and leukocyte stimulation.7
The blood-brain barrier has also been suggested to be affected by uraemia. This barrier is the only site that the TJ of the endothelium—and not epithelium— have been assessed. According to Hernandez et al, circulating toxins enter the brain circulation, resulting in neurological complications such as dementia, cognitive impairment, increased risk of stroke, retinopathy.8,9
TJ are complex proteinic structures located at the upper intercellular clefs of the epithelial cells and to a lesser extent, in the endothelium. They maintain the integrity of the paracellular barrier, and they also regulate the cell polarity by restricting the movement of membrane protein. They consist of three different protein teams, namely the transmembrane (occludin and claudin), the cytosolic (zonula occludens) and the peri-junctional (actin and myosin).4
The aim of our study is to evaluate the expression of the main TJ proteins at the endothelium (arteries and veins) of ESKD patients. This will be a prospective, single-centre, quadruple-arm, non-randomised interdisciplinary proof-of-concept study involving 100 patients. There will be 50 ESKD (Group 1) and 50 non-ESKD (Group2) patients. Subjects’ recruitment is shown in Figure 1.
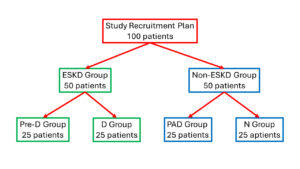
The ESKD group will consist of 25 pre-dialysis patients (Pre-D-group) and 25 dialysis patients carrying a dialysis catheter (D-group). In both groups tissue samples will be collected during scheduled arteriovenous fistula creation from the site of the anastomosis. The non-ESKD group will consist of 25 peripheral arterial disease patients (PAD-group) scheduled to undergo amputation, suffering common comorbidities with ESKD patients, without kidney dysfunction. The other 25 specimens will be collected from healthy vessels (no-comorbidities, no ESKD) from patients scheduled for nephrectomy. (Nephrectomy-group). Venous sampling will take place to all patients to evaluate different biomarkers.
The aim of the non-ESKD group is to evaluate the condition of TJ in patients without uraemia and that comorbidities do not affect expression of TJ proteins. In the ESKD group the different sub-cohorts aim to evaluate whether dialysis maybe a triggering factors influencing TJ protein expression.
Specimens will undergo a histopathologic assessment. To quantify the proportion of the TJ within the specimens, an immunohistochemical examination will be performed.
Nikos Giannikas is an interventional radiology resident at the University Hospital of Patras and head of the organising committee of the Endo Vascular Access (EVA) meeting. Panos Kitrou is an associate professor in interventional radiology at Patras University Hospital and director of the EVA meeting.
References:
- Lee T, Chauhan V, Krishnamoorthy M, et al. Severe venous neointimal hyperplasia prior to dialysis access surgery. Nephrol Dial Transplant. 2011;26(7):2264-70.
- <2015. Chronic kidney disease alters vascular smooth muscle cell phenotype.pdf>.
- Lee T, Roy-Chaudhury P. Advances and new frontiers in the pathophysiology of venous neointimal hyperplasia and dialysis access stenosis. Adv Chronic Kidney Dis. 2009;16(5):329-38.
- Lee DBN, Huang E, Ward HJ. Tight junction biology and kidney dysfunction. American Journal of Physiology-Renal Physiology. 2006;290(1):F20-F34.
- Vaziri ND, Yuan J, Norris K. Role of urea in intestinal barrier dysfunction and disruption of epithelial tight junction in chronic kidney disease. Am J Nephrol. 2013;37(1):1-6.
- Georgopoulou GA, Papasotiriou M, Bosgana P, et al. Altered Expression of Intestinal Tight Junctions in Patients with Chronic Kidney Disease: A Pathogenetic Mechanism of Intestinal Hyperpermeability. Biomedicines. 2024;12(2).
- Vaziri ND. Gut microbial translocation in the pathogenesis of systemic inflammation in patients with end-stage renal disease. Dig Dis Sci. 2014;59(9):2020-2.
- Hernandez L, Ward LJ, Arefin S, et al. Blood-brain barrier and gut barrier dysfunction in chronic kidney disease with a focus on circulating biomarkers and tight junction proteins. Sci Rep. 2022;12(1):4414.
- Toyoda K. Cerebral small vessel disease and chronic kidney disease. J Stroke. 2015;17(1):31-7.