Humacyte has announced positive top-line results from the V007 Phase 3 clinical trial of the acellular tissue engineered vessel (ATEV) in arteriovenous access for patients with end-stage renal disease. It stated in a press release that the ATEV demonstrated superior function and patency at six and 12 months (co-primary endpoints) compared to autogenous fistula, which is the current standard of care for haemodialysis patients.
Humacyte has announced positive top-line results from the V007 Phase 3 clinical trial of the acellular tissue engineered vessel (ATEV) in arteriovenous access for patients with end-stage renal disease. It stated in a press release that the ATEV demonstrated superior function and patency at six and 12 months (co-primary endpoints) compared to autogenous fistula, which is the current standard of care for haemodialysis patients.
The Phase 3 trial is a prospective, multi-centre, randomised clinical study in 242 haemodialysis patients in the USA. Enrolled individuals were randomly assigned to receive either the ATEV or an arteriovenous (AV) fistula for haemodialysis access and are being followed for up to 24 months. Under the statistical analysis plan for the trial, the primary efficacy assessment compared functional patency (usability for haemodialysis access) at six months and secondary patency (blood flow through the conduit) at 12 months, as co-primary endpoints. At six months, 81.3% of the patients implanted with the ATEV had functional patency compared to 66.4% of the patients receiving an AV fistula. At 12 months, 68.3% of the patients implanted with the ATEV had secondary patency, compared to 62.2% of the patients receiving an AV fistula. The joint test for superiority of the ATEV versus AV fistula at six and 12 months was statistically significant. Patients on ATEV also achieved a significantly longer duration of haemodialysis over the first 12 months, as compared to autogenous fistula. More adverse events were reported in patients on the ATEV treatment arm than those on the AV fistula treatment arm.
According to Humacyte, nearly 808,000 Americans are currently living with end-stage renal disease, requiring either dialysis or a kidney transplant, but the current standard of care for establishing access for haemodialysis has significant risks and shortcomings. It states that catheters, which are tunnelled underneath the skin, have high rates of bloodstream infection, while autogenous AV fistulas often fail to function, particularly for women, forcing patients to rely on infection-prone catheters. In addition, many patients are not suitable candidates for AV fistula placement due to gender, small vessel anatomy, advanced age, obesity, or other comorbidities.
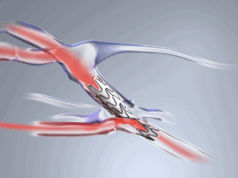
Humacyte’s ATEV is a bioengineered human tissue that it has designed to be a universally implantable vascular conduit for use in vascular replacement and repair, and for use as haemodialysis access. Humacyte stated in the press release that the ATEV has been observed to have a low rate of infection in clinical trials. The ATEV is designed to be available off-the-shelf, and ready whenever surgeons need it, potentially saving valuable operating room time and improving patient outcomes. As announced previously, based on guidance from the FDA, the proper or generic (non-brand) name “acellular tissue engineered vessel” (ATEV) has replaced the term “human acellular vessel” (HAV) that was previously used for our bioengineered vessel candidate.
Laura Niklason, chief executive officer (CEO) of Humacyte, shared their thoughts on the results, stating: “We are thrilled to announce positive results for the Phase 3 V007 trial, which we believe highlight the potential of the ATEV to improve AV access in haemodialysis patients who are underserved by the current standard of care. Achievement of this major milestone has taken a tremendous amount of effort and commitment from our patients, clinical investigators, employees, and other collaborators, and I thank them for their great support and contributions. We expect to discuss a potential market authorisation pathway for the ATEV in haemodialysis access with the Food and Drug Administration soon. We also look forward to presenting more detailed results from the study, including subgroup analysis results, at upcoming medical conferences.”