One-year results of the VENOS-1 first-in-human study, investigating the use of the Velocity (Venova Medical) percutaneous arteriovenous fistula (pAVF) system, have been published in the Journal of Endovascular Therapy.
In the paper, author Robert Shahverdyan (Vascular Institute, Hamburg, Germany) and colleagues write that the results of the 10-patient, prospective, single-arm, study demonstrate that an implant-based pAVF can consistently achieve physiologic maturation without the need for flow diversion from the deep venous system.
The study was designed to evaluate the safety and feasibility of the Velocity pAVF system, enrolling patients who were haemodialysis-dependent with a central venous catheter and had anatomy suitable for a surgical brachial-cephalic AVF.
Central venous catheters for chronic haemodialysis vascular access are a major source of morbidity and healthcare expenditure, the authors state in their paper, with shortening or avoiding central venous catheter contact time by creating long-term haemodialysis vascular access “a critical objective across healthcare systems”.
“There is broad consensus that a mature AVF is the preferred dialysis access due to its durability and improved patient outcomes. Nevertheless, over 80% of patients in the USA initiate haemodialysis with a central venous catheter notwithstanding decades of concerted effort to avoid central venous catheters, reflecting persistent barriers to permanent vascular access creation,” they write. Further to this delayed and incomplete AVF maturation may necessitate additional interventions, adding to and prolonging catheter dependence.
pAVF technologies offer promise in overcoming some of these challenges by addressing several procedural barriers, with Velocity designed to closely replicate surgical AVFs and to optimise flow within the superficial venous system.
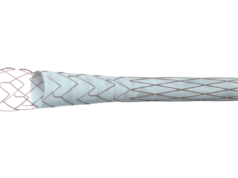
The device creates an AVF in the proximal forearm between the proximal radial artery and cubital perforating vein with an endovascular implant, allowing for upper-arm cannulation of the cephalic vein for patients requiring haemodialysis, the Journal of Endovascular Therapy paper details.

The implant is an expanded polytetrafluoroethylene (ePTFE)-covered nitinol frame with a fenestration for inflow, creating an end-to-side connection between the cubital perforating vein and the proximal radial artery, while simultaneously preserving unobstructed blood flow through the radial artery. The venous end of the implant diverts outflow from the multiple adjacent deep veins and delivers the totality of the access flow volume into the superficial venous system of the upper arm.
To test its technical feasibility and safety, investigators assessed the device against a primary effectiveness outcome of procedural success and primary safety outcomes of serious adverse device events and major reinterventions at six weeks. Secondary outcomes of the study included physiologic maturation, defined as brachial artery flow ≥500mL/min and venous outflow diameter ≥5mm, reintervention rate, and functional use.
The 10 patients included in the study had a mean age of 45 years and a mean body mass index (BMI) of 24.3kg/m2, with follow-up available out to an average of 15.9 months. All procedures were performed under an axillary block, with study subjects receiving acetyl salicylic acid (81mg) and clopidogrel (75mg) prior to the procedure and instructed to continue dual antiplatelet medications for three months.
All patients met the primary effectiveness endpoint, with intraprocedural duplex ultrasound used to confirm outflow from the proximal radial artery with no signs of arterialised blood flow into the deep venous system in any of the cases.
Brachial artery flow volume, which the study investigators describe as a key predictor of maturation and cannulation, increased progressively from 744mL/min at day one to 977mL/min at day 42. The study team reports a corresponding increase in upper-arm cephalic vein diameter from 3.4mm at baseline to 6.2mm at six weeks.
The composite outcome measure of physiologic maturation was achieved in all subjects, with a median time to achieving physiologic maturation of 18 days.
In the subsequent follow-up, one patient exited the study early due to catheter-associated sepsis at day 65 that colonised the implant, which was subsequently removed, however there were no infections in the remainder of subjects who were followed up through study termination.
Four subjects had split venous outflow through both basilic and cephalic veins and underwent ligation of the medial basilic vein to direct the flow toward the cephalic vein to facilitate inline cannulation, the investigators report, whilst nine patients achieved functional maturation with two-needle cannulation of the upper-arm cephalic vein, without the need for special training on cannulation technique.
“The pAVF access provided sustained clinical use over the duration of follow-up,” Shahverdyan and colleagues report. “There was a single balloon angioplasty of the venous end of the implant at 224 days in one subject, otherwise all other subjects have had uninterrupted functional use of the pAVFs throughout follow-up. The total number of reinterventions to maintain or restore access patency for all subjects was two over the course of the study, for an average of 0.2 reinterventions-per-patient-year. The access circuit primary patency at one year was 80% and cumulative patency was 90%.”
Though the implant-based pAVF reached the threshold for physiologic maturation, over the ensuing 12 months, brachial artery flow volume plateaued never exceeding 1,400ml/min, they note. The radial artery remained patent through the duration of the study for all subjects, with the flow in the radial artery retrograde or bidirectional in all patients, with no instances of thrombosis or occlusion. No instances of hand ischaemia or high-output pAVF were reported in any patient during follow-up.
“The results of this first-in-human study demonstrate the effectiveness of an implant-based approach for creating pAVFs for haemodialysis vascular access,” the study’s authors write in their discussion of the findings. “Beyond achieving 100% technical success and demonstrating a favourable safety profile, this method of access creation consistently delivered rapid and reliable physiologic maturation, minimal reintervention to the implant, functional use that did not require special cannulation techniques, and sustained patency through 12 months. These outcomes address critical needs necessary to optimise dialysis access performance and have substantial potential to address significant problems related to haemodialysis access creation, initial clinical use, and durability.”
Venova Medical, the developer of the device, has initiated two separate US prospective multicentre investigational device exemption (IDE) studies—VENOS-2 and VENOS-3—designed to provide further evidence of the safety and efficacy of the Velocity system. VENOS-2 began enrolment in January 2025 and will enrol up to 25 subjects at six US sites. VENOS-3 began enrolment in October 2025.
Shahverdyan first reported the one-year findings of the VENOS-1 study at the Controversies in Dialysis Access (CiDA) meeting in 2024 (3–5 October, Washington DC, USA).