VentureMed Group, a privately held medical device innovator in access management for arteriovenous (AV) fistulas and grafts and vessel preparation for interventional treatment of peripheral arterial disease (PAD) announced data presented at the VEITHsymposium, (15–19 November, New York, USA). Overall, the data presented demonstrated that Flex vessel prep used prior to balloon angioplasty improves 12-month outcomes both in PAD and AV fistulas and grafts.
VentureMed Group, a privately held medical device innovator in access management for arteriovenous (AV) fistulas and grafts and vessel preparation for interventional treatment of peripheral arterial disease (PAD) announced data presented at the VEITHsymposium, (15–19 November, New York, USA). Overall, the data presented demonstrated that Flex vessel prep used prior to balloon angioplasty improves 12-month outcomes both in PAD and AV fistulas and grafts.
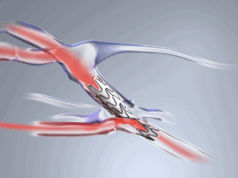
“AV Access management is a critical component of successfully treating AV patients over time,” said John Aruny (Dialysis Access Institute, Orangeburg, USA), primary investigator of the Flex Vessel Prep AV registry clinical study, the 12-month outcomes of which he presented at VEITH. “The FLEX AV Registry 12-month outcomes shows that utilising Flex vessel prep provides more time between interventions and continues to excel in the very difficult cephalic arch lesions.”
The study was a single arm, prospective study conducted in eight centres in the USA with 114 real world patients.
The Flex AV Registry 12-month outcomes demonstrate sustained patency across most patients and particularly good results specifically in the cephalic arch.
- 49% patency for all AV fistula patients (comparable historical data 26%)
- 59.7% patency for cephalic arch lesions (comparable historical data 0–33.9%)
- AV grafts had average time to target lesion revascularisation of 228 days (41.2% patency at nine months)
- No observed serious adverse events.
“Vessel preparation has become a necessary step for better patient outcomes,” said Eric Secemsky, director of vascular intervention, Beth Israel Deaconess Medical Center (Boston, USA), who presented the 12-month results of the Belong study with Flex vessel prep system prior to drug-coated balloon (DCB). “Vessel preparation in PAD with Flex creating longitudinal microincisions prior to DCB therapy had impressive freedom from clinically driven target lesion revascularisation and looks to improve outcomes by lowering balloon inflation pressures and potentially enhancing drug delivery.”
The Belong study was a single-centre, single-arm, prospective study conducted with 41 patients in Fribourg, Switzerland.
12-month efficacy results:
- 97.5% (39/40) freedom from clinically driven target lesion revascularisation
- 84.2% (32/38) freedom from target lesion restenosis via duplex
- 14/32 patients had stents
- 100% freedom from major amputation.