This advertorial is sponsored by Xeltis.

An de Vriese (Bruges, Belgium), who is playing a leading role in an ongoing European trial investigating the aXess vascular graft, discusses the study and the significant potential held by this technology in dialysis access care.
AZ Sint-Jan Brugge-Oostende AV (Bruges, Belgium) is one of the implanting centres in the new AXESS European pivotal trial of aXess—a novel, restorative, bioresorbable polymer-based vascular access graft for haemodialysis patients. Our centre had positive preliminary experience with the aXess graft, which we implanted in five patients, as part of the AXESS first-in-human (FIH) trial that recently completed enrolment. The novel structure and mechanical properties of this new device offer promise to overcome the limitations of current graft options, while over time acquiring similar properties to those of a native fistula. This could fulfil a major unmet need in haemodialysis vascular access.
An unmet clinical need
End-stage kidney disease (ESKD) patients requiring haemodialysis are exponentially increasing in number worldwide.1 The economic burden is sizeable, with costs of up to US$100,000 per haemodialysis patient annually.2 Current options for vascular access still entail high complication rates. Arteriovenous fistulas (AVFs) remain the preferred access for haemodialysis patients—the so-called ‘fistula-first’ treatment strategy—while arteriovenous grafts (AVGs) are generally considered a second-line approach3 due their inferior primary and secondary patency rates, and incidence of interventions and complications.4 However, the long mean time to AVF maturation (3.5 months) and the low success rate (26% at six months)5 led the 2019 Kidney Disease Outcomes Quality Initiative (KDOQI) vascular access guideline update to shift away from fistula-first, in favour of the ‘right access’ approach.6 Now, alternative solutions are very much in clinical demand.
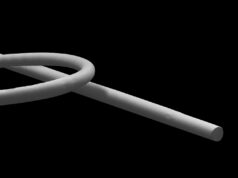
 The Xeltis haemodialysis access graft, aXess, is a novel, restorative, bioabsorbable implant made of electrospun supramolecular polymers. The device essentially allows the body to heal itself. Immediately after implantation, it acts as a functional haemodialysis AVG and, over time, provides a mechanical and structural scaffold for cell ingrowth propelled by the body’s natural healing process. The result is a living vessel with pluricellular components, including myofibroblasts and endothelial cells. The aXess graft enables immediate cannulation, potentially better patency rates, lower bleeding times after needle removal, and lower access site infection rates, compared to commercially available AVGs.
The Xeltis haemodialysis access graft, aXess, is a novel, restorative, bioabsorbable implant made of electrospun supramolecular polymers. The device essentially allows the body to heal itself. Immediately after implantation, it acts as a functional haemodialysis AVG and, over time, provides a mechanical and structural scaffold for cell ingrowth propelled by the body’s natural healing process. The result is a living vessel with pluricellular components, including myofibroblasts and endothelial cells. The aXess graft enables immediate cannulation, potentially better patency rates, lower bleeding times after needle removal, and lower access site infection rates, compared to commercially available AVGs.
Assessing the aXess graft
The clinical trial evaluation of the aXess graft started with the AXESS FIH trial (NCT04898153)—a single-arm, prospective, multicentre trial assessing safety and effectiveness of the device. In this trial, 20 patients were successfully enrolled in six European sites, including ours, between June 2021 and September 2022. Promising preliminary results were presented earlier this year at the Charing Cross (CX) Symposium (26–28 April, London, UK) and more recently at the Porto Vascular Conference (7–8 October, Porto, Portugal). Full cohort data are expected in 2023.
Following very promising early clinical outcomes, study sponsor Xeltis has now initiated the AXESS EU pivotal trial (NCT05473299) as a go-to-market multicentre trial. Primary endpoints include freedom from device-related serious adverse events and primary patency at six months. The objective is to enrol 110 patients at up to 25 European sites and follow up with them for five years. The initiation of a pivotal trial for the aXess graft is promising for the future of haemodialysis vascular access, as its core technology may potentially combine the optimum characteristics of currently available options to offer patients, physicians and payers a solution for a major unmet need.
References:
- Thurlow J S, Joshi M, Yan G et al. Global Epidemiology of End-Stage Kidney Disease and Disparities in Kidney Replacement Therapy. Am J Nephrol. 2021; 52(2): 98–107. doi: 10.1159/000514550.
- Swaminathan S, Mor V, Mehrotra R et al. Medicare’s payment strategy for end-stage renal disease now embraces bundled payment and pay-for-performance to cut costs. Health Aff (Millwood). 2012; 31(9): 2051–8.
- Murea M, Geary R L, Davis R P et al. Vascular access for hemodialysis: A perpetual challenge. Semin Dial. 2019; 32(6): 527–34.
- Almasri J, Alsawas M, Mainou M et al. Outcomes of vascular access for hemodialysis: A systematic review and meta-analysis. J Vasc Surg. 2016; 64(1): 236–43.
- Bylsma L C, Gage S M, Reichert H et al. Arteriovenous Fistulae for Haemodialysis: A Systematic Review and Meta-analysis of Efficacy and Safety Outcomes. Eur J Vasc Endovasc Surg. 2017; 54(4): 513–22.
- Lok C E, Huber T S, Lee T et al. National Kidney Foundation. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis. 2020; 75(4 Suppl 2): S1–S164.
An de Vriese is the head of Nephrology and Infectious Diseases at AZ Sint-Jan Brugge-Oostende AV in Bruges, Belgium, and coordinating investigator of the AXESS EU pivotal trial.