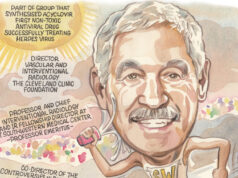
With a career spanning 60 years, a passion for music and photography, and a wealth of experience in teaching and leading the future clinicians of his field, clinical professor at University of Texas Medical Branch (Galveston, USA) Gerald Beathard speaks to Renal Interventions about his career in interventional nephrology (IN), those that helped him at the beginning of his career and what he feels the future of IN should look like.
With a career spanning 60 years, a passion for music and photography, and a wealth of experience in teaching and leading the future clinicians of his field, clinical professor at University of Texas Medical Branch (Galveston, USA) Gerald Beathard speaks to Renal Interventions about his career in interventional nephrology (IN), those that helped him at the beginning of his career and what he feels the future of IN should look like.
What drew you to a career in IN?
I more or less eased into it over time. I didn’t really think that I was going to engage in a career in IN, but in taking care of dialysis patients in the late 1970s, I was encountering patients who had problems with their vascular access, and nobody seemed to understand what the problem was. This also meant that no one was really addressing it directly. If a patient had a problem with their vascular access, the general approach was that the surgeon would revise it or create a new access.
However, in the 1980s, there was an article published that discussed doing balloon angioplasty on venous structures; prior to that, balloon angioplasty had only been on arteries. It reported angioplasty results on venous structures—some of which were dialysis access—which piqued my interest. I said “that maybe something like that can be done”, and from that I decided that I would start doing angiograms on our patients, by taking regular X-rays of patients with contrast injections, with the needles in place.
Around this time, a cardiologist joined our clinic who was willing to help me start doing dialysis access angioplasties. He called me one day and said that he was going to an arterial angioplasty course and asked if I would like to go. The one-day course consisted primarily of lectures, with a live video demonstrating the technique at the end of the course. Everyone was given a certificate that said we were now qualified to do femoral artery angioplasties. I’d never done one, but I had a certificate that said I was qualified to do it. I came back and applied to the credentials committee to start performing angioplasties on dialysis access, with this cardiologist as my proctor. He showed up for the first case and stayed for a few minutes, and that’s the last time I saw him. After that, I started treating venous outflow stenosis with angioplasty on a regular basis.
Did you have any mentors that helped you during your career?
Early on, the only people that I could say served as mentors were the radiology technologists who worked in interventional radiology where I was doing cases. There was no one that I could turn to that had any experience in handling these kinds of cases. The radiology technologists would tell me what the interventional radiologists were doing, what kind of balloons and guidewires they were using. Along with their guidance, it was more or less trial and error. I did make a few mistakes—nothing major—but I collected data on every case that I did. I also attended a one-day course on dialysis access thrombectomy, after which I started doing thrombectomies.
In Texas, we had a small, informal association of nephrologists, which paid a small fee for Allen Hull (Dallas, Texas) to serve as a lobbyist in Washington, and to represent us in issues involving the Centers for Medicare & Medicaid Services (CMS). At one point, I received a bulk mail-out from CMS implying that they would not pay for venous angioplasty on dialysis access. I contacted Hull regarding this, and he told me that he wasn’t familiar with the procedures that I was doing on dialysis access and that he would check with some associates and get back to me. He later said that those he had spoken to were not familiar with what I was doing and were sceptical as to its value, despite what I had found. He replied that I needed to write a paper reporting my results, providing evidence of its value. Using the data I had collected, I wrote a paper reporting on about 300 cases, and continued performing dialysis access procedures with no reimbursement issues.
 What do you think is the most important thing to develop for the next 10 years of IN?
What do you think is the most important thing to develop for the next 10 years of IN?
I think that we’ve gone through a time where freestanding access centres, being operated by nephrologists, have been very important and extremely valuable to patient care. However, reimbursement has gotten to the point where many of these centres are not financially viable. It seems that IN is being forced to move into ambulatory surgical centres and hospitals. With this change, I think that the efficiency with which nephrologists were able to do these procedures is suffering. In the freestanding extension of office model, it was not unusual to see a nephrologist do 10–12 cases a day. Working in a hospital, it’s only possible to do less than half of that number. With reimbursement as it is, I think that it’s getting to the point where it’s financially difficult for a nephrologist to practice IN.
I feel that, going forward, we need to develop dedicated centres that can offer the full spectrum of services needed for dialysis access management. With this, we need to have practitioners—not nephrologists necessarily—that can offer the complete range of what is needed for vascular access care in a dialysis centre, ranging from ultrasound evaluation all the way up through surgery. Some centres offer that now; in some instances, this is a single physician, and in others, there are several practitioners—some of them nephrologists, some are surgeons, and some of them are interventional radiologists. I think the future of vascular access is moving in that direction.
You have been referred to as one of the “founding fathers” of the American Society of Diagnostic and Interventional Nephrology (ASDIN). What do you think have been some of the bigger achievements as a society?
One of our big achievements is the high quality of interactive meetings that we have recently had (23–25 February 2024, New Orleans, USA) as a society, that has actually become multidisciplinary. When we first started, our meetings were relatively small, and we generally had them in conjunction with either the American Society of Nephrology or the American Kidney Foundation, discussing subjects that were really very basic. Today, we have much more complicated issues being discussed and, crucially, our meetings have become multidisciplinary. If you look at the speaker agenda from our recent annual meeting, we had radiologists, surgeons, and interventional nephrologists on the schedule, as well as nephrologists. We have also expanded so that we have nurses and an associates meeting, for practitioners who are vital to the care of dialysis patients. I think that this type of meeting has been, in my mind, a major accomplishment. Much of this can be attributed to our executive secretary, Mary Lea Nations, who has really done a Herculean job.
The other major issue is the offering of a specialty certification. We have not been able to get the American Board of Medical Specialities to offer certification for IN because they say that the numbers are not large enough to make it financially feasible. However, it’s often essential for a physician to have some type of certification in order to get the necessary practice credentials. The society has developed a robust certification and recertification system to offer this type of recognition.
What advice would you give someone looking to move into the field of IN?
They need to be associated with a programme that is offering this training at a high level of clinical expertise. Unfortunately, there are only a few IN training programmes available. They also need to have a good general nephrology training programme, because most interventional nephrologists also practise a significant amount of general nephrology as well. Radiologists and surgeons also need to have training from someone that can give them the type of insights that they need to understand dialysis, the literature, and also how to do these procedures appropriately. If you take something as simple as putting in a dialysis catheter, there are certain things that are not immediately obvious that need to be followed to do it appropriately. A surgeon or radiologist who just has basic training in their specialty is not going to be able to offer the high level of dialysis access management that the patient deserves.
How significant do you think that the patient experience should be in the future of IN?
I think the patient’s perspective is very important, and I think that it starts with making strong patient relationships. One of the things that’s happened in the past, that I’m afraid is going to be less of a feature going forward, is many of the interventional nephrologists have been doing procedures on the patients of their practice that they also see in their offices and in the dialysis unit. They have developed a close relationship with these patients. I think having that relationship, where the patient can have a sense of confidence in them as their physician, is extremely important. It’s important to really know the patient, to know things about the patient that may not be obvious, and things about their family and social situation. These things can have a significant effect on the patient’s quality of life. Many of the procedures that are performed are for problems that tend to be recurrent. You hope that it’s going to be quite some time in the future, but you’re probably going to see that patient again. I think that if the patient has one bad experience, it’s going to have a very unfavourable effect on the relationship between the physician and the patient. Unfortunately, it is also going to bleed over into other patients, because the patients in the dialysis unit tend to talk to other patients. I think having a very positive patient-physician relationship is critically important.
What are your interests outside of medicine?
I do a lot of medical writing, but I’m also very interested in outdoor and wildlife photography. I worked for a group called Lifeline—a subsidiary of DaVita—for almost 20 years, developing freestanding access centres around the country. Eventually, we had 78 centres, most of which were decorated with my photographs that I had printed, framed and hung myself. I like to cook and have attended cooking schools in China, Greece, Italy, and Portugal, as well as the USA. I also have a passion for music; I sing in a church choir, and was privileged to sing at both President and Barbara Bush’s funerals because they were held at the church I attend in Houston. That was quite an experience. I’ve also written and published more than 100 Southern Gospel songs.
Fact file
Current appointment:
Clinical professor, University of Texas Medical Branch, Galveston, USA
Education:
1960–64: Medical School: University of Texas Medical Branch, Galveston, USA
1964–65: Internship: University of Texas Medical Branch, Galveston, USA
Honours (selected):
1986: Physician of the Year 1986, Austin Diagnostic Clinic, Austin, Texas
1993: Brackenridge Hospital, Austin Texas Physician of the Year Award
2007: American Society of Diagnostic and Interventional Nephrology Lifetime Achievement Award
2008: Establishment of Gerald Beathard Excellence in Academic Achievement Award
2008: Establishment of Gerald Beathard Lectureship
2016: University of Texas Medical Branch Ashbel Smith Distinguished Alumnus Award
2021: Establishment of Gerald Beathard Outstanding Nephrology Fellow Award