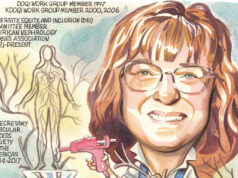
From beginning a career in medicine to collecting Agatha Christie’s works, professor of medicine at Emory University (Atlanta, USA) Vandana Dua Niyyar speaks to Renal Interventions about her career in interventional nephrology (IN), how she occupies her time between her various roles and cases, and those that have inspired, advised and guided her throughout her career. As president of the American Society of Diagnostic and Interventional Nephrology (ASDIN), she also shares her thoughts on the future of IN and the biggest challenges facing dialysis care.
From beginning a career in medicine to collecting Agatha Christie’s works, professor of medicine at Emory University (Atlanta, USA) Vandana Dua Niyyar speaks to Renal Interventions about her career in interventional nephrology (IN), how she occupies her time between her various roles and cases, and those that have inspired, advised and guided her throughout her career. As president of the American Society of Diagnostic and Interventional Nephrology (ASDIN), she also shares her thoughts on the future of IN and the biggest challenges facing dialysis care.
What drew you to a career in medicine and IN?
I guess you could say that it runs in the family. I was very young when I knew that I wanted to be a doctor. My parents are my lifelong role models and inspiration—my father is a doctor and my mom is a teacher. I have been extremely fortunate to be able to nurture their legacy by incorporating both their passions into my career in academic medicine as a clinician-educator.
As for IN, it was destiny. I was considering a career as a physician scientist, and as part of my extended research fellowship, I was in the process of applying for funding and writing multiple grants including a National Institutes of Health (NIH) Mentored Patient-Oriented Research Career Development Award programme (K23). In the penultimate month of my fellowship, my division chief asked me to spend a month at our access centre and to evaluate its merits as a rotation for second year fellows. I had no idea that in fact they were the ones who were evaluating me—for a faculty position as an interventional nephrologist! It turned out to be a win-win for both sides—from the very first day itself, I realised I loved it—the instant gratification of getting the flow and thrill back after a successful thrombectomy was exhilarating, and a welcome addition to the delayed gratification that you get after many years in research.
Looking back, I feel very lucky that I have had the opportunity to be able to incorporate all these different experiences into my career.
Has your role as the president of ASDIN led to any developments in IN that you are particularly proud of?
It has been my absolute honour to serve ASDIN as president for the last two years. We have an incredibly engaged membership and leadership whose passion and dedication to help us achieve our mission of optimising dialysis access care is inspiring. Together, we have forged a strategic plan and restructured our committees to not only bolster long-term foundational support, but also to provide sustainable future impact and success.
A few of the initiatives that are particularly close to my heart include the establishment of a patient perspectives committee that seeks to bring—for the first time in over 20 years— the patient voice to ASDIN, ensuring that the patient perspective serves as our true north. Our research committee has revamped our research grants and, in the pursuit and support of new knowledge, has initiated a mentoring programme.
As a passionate proponent of ultrasound, I am extremely proud of our comprehensive ultrasound certification programmes in three separate areas—renal ultrasound, dialysis access, and volume assessment—that were unveiled earlier this year and aim to bring the “D” (diagnostic) back in ASDIN. Our haemodialysis, vascular access, endovascular arteriovenous fistula (endo AVF) and peritoneal dialysis catheter (PD) certification processes have consistently maintained the delicate balance of establishing and enforcing stringent quality criteria that are essential to achieving and maintaining the high quality of care that our patients deserve.
ASDIN recognises how critical it is for all of us to work together across disciplines and as a global community, and share our knowledge and expertise with each other. We have expanded our outreach to multidisciplinary professionals including surgeons and frontline dialysis staff, as well as internationally through a multitude of educational offerings including ASDIN Global and our ASDIN-international society of nephrology (ISN) ultrasound webinars, while exploring further collaborations worldwide.
The field of dialysis access is rapidly evolving and ASDIN is uniquely positioned to harness this momentum through innovation and advancement. As president, it has truly been my privilege to be a part of this exciting journey and explore and expand upon the vast and diverse opportunities for collaborations in research, training and education.
What is the biggest question in IN that you would like to see answered?
Dialysis access is meant to be the patient’s lifeline, but more often than not, it tends to be their most vulnerable area—their Achilles’ Heel. For years, we have been describing the desired characteristics of what constitutes the “ideal” access but despite recent advances, have not yet been successful in achieving the lofty goal of an access that is durable and functional with minimal interventions and complications. I would like us as a community to take on this challenge, really listen to the patient and incorporate their perspective into future innovations, to design the next generation of dialysis access.
What do you think the next 10 years will look like for kidney care?
This is an exciting time to be a nephrologist. After many years of stagnation, the landscape in the management of kidney disease is rapidly changing, and for the better. For years, we had only renin-angiotensin system (RAS) inhibition as definitive targeted therapy to slow kidney disease progression but with the emergence of powerful new medications like sodium-glucose co-transporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists, we now have an unparalleled opportunity to change the trajectory of kidney disease. The optimists among us hope they will ultimately keep many of our patients from requiring renal replacement therapies. For those individuals suffering from kidney disease, in the future I foresee patient-centred personalised care that incorporates scientific and technological innovations to be the norm rather than the exception.
What, in your view, is the biggest roadblock to further developments in dialysis?
The kidney was the first solid organ whose function could at least be partially replaced by a machine, as well as the first to be successfully transplanted. It is fascinating to see how dialysis has evolved over the years. From the first machine developed by Dr. Willem Kolff using a wooden drum and cellophane casing, to the ubiquitous dialysis machines we see nowadays, clinical trials of the wearable artificial kidney in progress, and implantable bioartificial kidneys and cellular regeneration that are in preclinical stages, we have come a long way—but there is still a lot more to accomplish.
Dialysis as a way of replacing kidney function remains sub-optimal, as it focuses on solute and fluid clearance, but does not address the metabolic or endocrine functions of the kidney. Innovators are working across the board and combining forces to overcome the limitations of tissue engineering, miniaturisation, nanotechnology, and cellular regeneration in order to create a next-generation technology that would use a patient’s own cells to create a fully functional implantable organ. It is a work in progress and to quote Vincent Van Gogh: “As practice makes perfect, I cannot but make progress; each drawing one makes, each study one paints, is a step forward.” With time, I am confident that these roadblocks will be overcome and growth in this area will be exponential.
What is the best advice that you give your students who express an interest in pursuing IN as a specialty?
IN is a natural extension of our role as nephrologists and I encourage my students to be excellent nephrologists first, and then build on that foundation to develop expertise in the hands-on component of IN. I remind them to think beyond just the procedural component of IN and to remember that an interventional nephrologist is one who is a) committed to dialysis access, b) understands the complexities of the dialysis patient and the process of dialysis, and c) has expertise in the procedures required, as Gerald A Beathard (University of Texas Medical Branch, Galveston, USA) said. Interventional nephrologists, with their unique skillset, have a pivotal role to play in optimising care of the patient on dialysis, breaking down silos and work in tandem with the other professionals. They are uniquely positioned to be the best advocates for their patients, and the leaders of the multidisciplinary team taking care of this vulnerable patient population. Of course, compassion and intellectual curiosity are also a must for everyone in medicine.
What is your philosophy within medicine, particularly within IN?
I have always felt that medicine is not just a career, it is a calling. I live by the phrase “choose a job you love and you will never have to work a day in your life”. Medicine is truly my life’s passion and joy, and when I am with my patients, to be honest, it does not even feel like it is ‘work’.
As for the procedural component of IN, I will quote one of my mentor’s wise words: “The enemy of good is better.” It is not only essential to know when and how to perform a procedure, but even more important to know when to stop.
What are your interests outside of medicine?
Outside of medicine, I love spending time with my family, travelling all over the world, and exploring new places, cultures, and cuisines. While the kids were growing up, I focused only on my family and my work, but now that we are empty nesters, I have been able to rekindle some of my other interests.
I love reading—mostly fiction—I am a huge Agatha Christie fan and have a hard bound copy of every single title she has written! My current non-fiction favourites are Becoming by Michelle Obama and Born a Crime by Trevor Noah. I am a Bollywood aficionado, and I have recently started taking Bollywood dance classes. I spend a lot of time outdoors when I can, and love to capture the beauty of our world through my camera lens; I now have a very nice collection of nature photography.
Fact File
Current appointments:
Professor of Medicine, Division of Nephrology Emory University, Atlanta, USA
Consultant Nephrologist, Grady Memorial Hospital and Emory University Hospital, Atlanta, USA
President, American Society of Diagnostic and Interventional Nephrology (ASDIN)
Education:
1989–1994: Medical School: Pt BDS Post- Graduate Institute of Medical Sciences, Maharishi Dayanand University, Rohtak, Haryana, India. Dean: Dr S B Siwach, MD
1994–1995: Internship: Pt BDS Post-Graduate Institute of Medical Sciences, Maharishi Dayanand University, Rohtak, Haryana, India, Dean: Dr S B Siwach, MD
Honours (selected):
2019: Distinguished Service Award, American Society of Diagnostic and Interventional Nephrology
2019: Woodruff Leadership Academy
2019: Nanette Wenger Distinguished Service Award Emory DOM
2020: Distinguished Clinical Service Award, American Society of Nephrology (ASN)
2021: Eminent Physician, Emory School of Medicine (SOM)
2021: Clinical Excellence Award, American Nephrologists of Indian Origin
2022: Outstanding Quality Achievement Award, Emory Department of Medicine