A new study in the Journal of Vascular Access (JVA) has found that, while arteriovenous fistulas (AVFs) that do not require assistance to mature have the best outcomes in the long term, unassisted arteriovenous grafts (AVGs) demonstrate better outcomes than assisted AVFs. The investigation was led by Muhammad Saad Hafeez (University of Pittsburgh Medical Center, Pittsburgh, USA).
A new study in the Journal of Vascular Access (JVA) has found that, while arteriovenous fistulas (AVFs) that do not require assistance to mature have the best outcomes in the long term, unassisted arteriovenous grafts (AVGs) demonstrate better outcomes than assisted AVFs. The investigation was led by Muhammad Saad Hafeez (University of Pittsburgh Medical Center, Pittsburgh, USA).
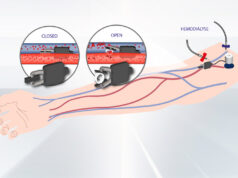
Hafeez and his co-authors state in their introduction that AVGs are generally associated with worse function after maturation despite their being cannulated “more reliably” than AVFs and often requiring “fewer maturation procedures to obtain functional patency”. Their study sought to provide clarity around the outcomes after maturation in AVFs and AVGs, while also further stratifying by patients who did and did not need maturation assistance procedures for each of the access types.
The study was a retrospective analysis utilising data from the US Renal Data System covering the period from 2012 to 2017. From these data, patients designated for inclusion were those who began dialysis with a central venous catheter before undergoing either AVF or AVG placement, and achieved successful two-needle cannulation. Sub-hazard ratios (sHR) were calculated according to rates of primary patency and access abandonment following maturation in the patient data.
Among the selected patients, who numbered 54,999, 42,664 received an AVF and 12,335 an AVG. Interventions were required for maturation in 18,408 of the AVF patients (43.2%) compared with 2,594 of AVG patients (21%; p<0.01). The study authors also point out that patients receiving assisted AVG—as well as assisted AVF—“experienced patency loss at one year more frequently” compared with unassisted AVG, 67.5% for assisted AVG, 57.5% for assisted AVF and 55.2% for unassisted AVG. The lowest rate of patency loss, which was 38.9%, was seen with unassisted AVF.
The authors add that the trends were “robust on adjusted analysis”, outlining the analysis results as follows: unassisted AVG reference, assisted AVG sHR=1.44, p< 0.01; assisted AVF sHR=1.08, p< 0.01, unassisted AVF sHR=0.67, p< 0.01. They also found that assisted AVGs were more likely to be abandoned (17.2%) than unassisted ones (11.7%).
Reviewing the findings in their conclusion, the authors state that unassisted AVFs “have the best long-term outcomes,”, but that primary patency is lost more quickly with assisted AVF than unassisted AVG. Putting forward some applications of their findings, they also suggest that AVG may be preferable over AVF “if veins are marginal and likely to require assisted maturation”. They do add, however, that more investigations are required to uncover the “anatomic and physiologic factors” affecting the outcomes associated with different access types, and which “influence conduit choice”.
Senior author Theodore H Yuo (University of Pittsburgh School of Medicine, Pittsburgh, USA) told Renal Interventions: “When ESKD patients have excellent venous and arterial anatomy for a native arteriovenous fistula, they are best served by undergoing creation of such an access. However, many patients exhibit suboptimal anatomy, and their AVF will likely require interventions to obtain functional patency. In those cases, our study suggests that compared to AVF, an AVG may have equal long term performance with the advantage of shorter time to cannulation. This highlights the importance of personalising medical care to the individual patient.”