Peritoneal dialysis (PD) is often foreshadowed by the dual spectre of fear of infection and peritonitis. “This happens because many nephrologists only see complications when patients are admitted [into hospital] and not the many fit patients in the community. In fact, PD infection rates are no different to haemodialysis (HD) and are often less consequential,” Edwina Brown, president of the International Society for Peritoneal Dialysis (ISPD) and professor of Renal Medicine, Imperial College London (London, UK), tells Renal Interventions.
Peritoneal dialysis (PD) is often foreshadowed by the dual spectre of fear of infection and peritonitis. “This happens because many nephrologists only see complications when patients are admitted [into hospital] and not the many fit patients in the community. In fact, PD infection rates are no different to haemodialysis (HD) and are often less consequential,” Edwina Brown, president of the International Society for Peritoneal Dialysis (ISPD) and professor of Renal Medicine, Imperial College London (London, UK), tells Renal Interventions.

The ISPD is running a joint session with the UK Kidney Association at the latter organisation’s annual meeting, UK Kidney Week (UKKW; 11–13 June, Edinburgh, UK), on improving the quality of life for older people having dialysis. Brown outlines the “patchy” global usage of PD and takes aim at the multiple forces that are obstacles to improving this modality’s uptake.
What is the vision for the ISPD session at UKKW on improving the quality of life for older people having dialysis?
We aim to increase awareness of the need to think about and offer PD to older people, particularly when they are frail and/or have cognitive impairment. Vitally, we believe that with assistance, older people can have PD at home. Older, frail people find HD exhausting, and transport to the HD unit crushing. One of the most important things that older people are frightened of is the development of dementia; there is a need to discuss the risk of rapid deterioration in cognition on HD, particularly now with hard evidence of drops in cerebral blood flow and brain injury on HD.
Could you provide a succinct snapshot of how home HD therapies are being used in the global setting, particularly PD?
Very simply, the use of PD is patchy. In Europe, this can range anything from <5% in most of Eastern Europe, and even in Germany and France, to more like 25–30% in Scandinavia. Home HD use is even lower.
What are your main arguments that PD is a good option for frail and elderly end-stage kidney disease (ESKD) patients?
When on PD, the person is in their own home, or nursing home, and not dependent on transport. The time to recovery after HD is longer in older and frail people, and the risk of hypotension on HD with associated drops in cerebral blood flow, myocardial stunning, or loss of kidney function well documented. Older people usually start dialysis with residual kidney function so do not need a full dose of dialysis, which corresponds often to only two or three exchanges, five or six days per week. Residual kidney function declines more slowly with increasing age and on PD compared to HD so these people often stay on low dose for their remaining lifespan. Many older people cannot perform their own dialysis but can be assisted by families and/or by paid assistants. This is still cheaper than in-centre HD when the cost of transport is added in, particularly when complex transport, for instance an ambulance plus a stretcher, is added in. Either automated peritoneal dialysis (APD) or continuous ambulatory peritoneal dialysis (CAPD) can be used, but many older people do not want to be attached to machines because of anxiety and/or wandering at night, particularly if there are cognition issues.
PD—or any sort of dialysis—is only one part of care for an older person requiring dialysis. People on dialysis have accelerated ageing, and age-related syndromes should be recognised and managed in collaboration with geriatric and palliative care teams. Being on PD enables people to access support systems in the community—many of which are excellent.
What are the most important obstacles to PD, which result in this option being overlooked or underused?
There is, unfortunately, both bias against use of PD and lack of knowledge. It’s clear there is a vicious cycle that operates beginning with bias against PD (for a variety of reasons) that leads to low use, and therefore there is a lack of expertise that develops and also a lack of knowledge and failure to develop support pathways such as PD catheter placement, surgery, microbiology that all contribute to poor outcomes when a patient is put on PD, and yes, this again then increases the negative bias.
What education is needed in the kidney care community to overcome these barriers?
There is a real need for general education about PD to all members of the renal team, making available knowledge and the choice of PD to all patients starting dialysis. Time in a PD unit, attendance in PD clinics and PD-related courses should be compulsory parts of nephrology training. Management also needs to be aware of the advantages of PD in terms of cost benefits: fewer nurses, better patient satisfaction, lower costs overall, so that care pathways are developed and supported.
What are the main issues that “plague” the idea of PD? Are these backed by evidence and how can outcomes be optimised in different countries and healthcare settings?
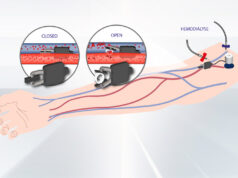
PD is haunted by the fear of infection and peritonitis. This happens because many nephrologists only see complications when patients are admitted [to hospital] and not the many fit patients in the community. In fact, PD infection rates are no different to HD and are often less consequential. The other issue is the availability of PD catheter insertion. PD happens more often when nephrologists can insert catheters percutaneously and are therefore not totally dependent on surgeons. A global issue, and fortunately not one in UK, is privatisation of HD with higher reimbursement for nephrologists compared to PD, because they see patients thrice a week on HD but probably only about once a month when they are receiving PD. And in the crossfires of this issue, in some countries nephrologists own HD units or get an incentive or a ‘bribe’ when a patient starts on HD.
Is there any new evidence that the renal care community needs to be aware of?
Front and centre should be an increasing awareness of the global nursing crisis. There is also emerging evidence about sustainability, with PD being environmentally ‘greener’ than HD. Of course, there is the predicted continued growth of the ESKD population which will overwhelm HD centres in many countries and the overarching limitation in healthcare resources and costs in all countries. These are all factors that need to be taken into account.
What would you say to patients and the teams that care for them to influence them to look at PD as a worthy approach?
When talking to patients who will need dialysis, I urge physicians and teams to tell each person there are two ways of doing dialysis; the first is coming to a hospital/renal centre three times every week or having a treatment at home. The first response to this from most patients is: ‘at home’. No one wants to go to a hospital three times a week. The next step is to assess feasibility and establish what the barriers are. There are very few absolute barriers against dialysis at home—most can be overcome with a bit of imagination. Several surveys polling the wishes of healthcare teams reveal that if they or their relatives had to have dialysis, 80% or so would always choose dialysis at home. We should clearly be offering the same to our patients.
What are some of the initiatives underway to help augment the use of PD?
NHS England aims to have a prevalence of home dialysis of 20% of all dialysis—this requires a much higher incidence rate. Regional kidney networks are therefore promoting steps to increase use of home dialysis, and these will vary in different regions. The availability of assistance has a big impact on people being able to start on PD, and to remain on PD. This becomes especially important when they are no longer able to do their own dialysis, or family members are no longer available, for instance if a daughter or son gets married or a spouse falls ill. ISPD has just published a position paper stating that assisted PD is an essential component of PD delivery; this should enable units to access and develop assistance, if they are not doing so already.