A systematic review published in the Journal of Vascular Access (JVA) has illuminated haemodialysis patients’ views and experiences of arteriovenous access cannulation, concluding that many patients learn to tolerate its unpleasantness out of a sense of necessity, with feelings of safety and control over the procedure often helping to facilitate this.
“Patients learn to survive repetitive cannulation, where feeling safe and in control can improve their experiences,” Catherine Fielding (University Hospitals of Derby and Burton NHS Foundation Trust, Derby, UK) and colleagues write in their JVA report. “This indicates cannulation is not just a technical skill, but also a social process. Cannulators and haemodialysis environments need to make patients feel safe and in control.
“Cannulation techniques may also influence these aspects, but further research is needed to determine how. Whilst this review has helped further develop our understanding about patients’ experiences of cannulation for haemodialysis, there is still much to understand about this phenomenon, to continue to improve this for haemodialysis patients.”
Fielding and colleagues begin by noting that cannulation is an essential part of haemodialysis—yet patients’ experiences are problematic and poorly understood. As such, they set out to assess the existing literature in this space, conducting a qualitative systematic review to synthesise studies that explore patient experiences of cannulation, vascular access (VA) and haemodialysis.
Eligible studies included those pertaining to a population of patients with end-stage kidney disease (ESKD) within the context of both in-centre and home haemodialysis. The authors note that databases including MedLine, CINAHL, EMBASE, EMCARE, BNI, PsycInfo and PubMed were last searched between 20–23 May 2019 to obtain these studies, while meta-aggregation was used to synthesise the resultant findings.
The database search, they detail, identified 246 eligible studies. Following the removal of duplicates and two stages of screening, a total of 26 studies were included in the final analysis. “Only four studies were directly about cannulation,” Fielding and colleagues report. “Other studies were about pain, experiences of VA for haemodialysis, experiences of in-centre and home haemodialysis, and research priority setting.” They also note that included studies were conducted across five continents.
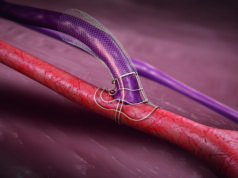
Regarding the content and findings of these studies, the authors identified three key themes and 10 sub-themes on patients’ experiences of cannulation. “Cannulation creates unpleasant feelings and is not a normal procedure for patients to experience regularly,” Fielding and colleagues write, discussing the first of these three overarching themes. “Cannulation for haemodialysis is associated with pain, concern about the abnormal appearance of the arteriovenous access, vulnerability and dependency. The context of regular haemodialysis makes this a unique procedure that is not similar to other one-off cannulation events.”
In addition to the unpleasant and unique nature of cannulation for these patients, the second major theme identified by the authors is the fact it is something of a necessary evil in haemodialysis—and patients themselves are accepting of this. This link to a life-sustaining and essential treatment changes what cannulation success means, they add, and leads to additional worry over whether it will be successful.
Drilling down further into the patient perspectives on the definition of successful cannulation, Fielding and colleagues state that easier needle insertion and reduced pain during cannulation—as well as the absence of pain throughout dialysis treatment—were found to be defining factors. They also report that patients viewed difficult cannulation as having a direct and negative impact on the effectiveness of their haemodialysis treatment, and held worries over damage to their arteriovenous access following difficult cannulation.
The third and final theme identified by the authors is the role necessity and regularity of cannulation for haemodialysis play in helping patients to overcome, or at least endure, these procedures. They report in JVA that patients often learn to tolerate, or become used to, cannulation. Feeling safe—a factor influenced by the environment in which it is conducted, the cannulation technique used, and even the patient’s relationship with and level of trust towards their cannulator—was found to influence patients’ ability to tolerate the procedure, as was their capacity to exert some control over the cannulation. On this front, self-cannulation was found to provide a sense of achievement, creating independence and self-efficacy, despite being associated with its own challenges.
“Finally, not all patients were able to cope with the unpleasantness of cannulation, leading to some avoiding cannulation,” Fielding and colleagues add. “Some did this by reducing the frequency of haemodialysis…others felt ‘it would be easier to do it having line access because of the way that the hookups work’. However, where possible, some patients completely avoid haemodialysis due to thoughts of the cannulation.”
Discussing their findings, the authors note that, overall, the necessity of cannulation and its link to life-sustaining haemodialysis treatments contributes to a “heavy burden” for patients, and concern over miscannulation is central to this. “Whilst preventing miscannulation is the optimal solution, it is unlikely that it can be avoided completely,” Fielding and colleagues add. “Therefore, better strategies are also needed to support patients through miscannulation.”
Regarding potential improvements to this state of affairs, they go on to state that cannulators, but also managers who influence nursing schedules and workloads, should “aspire to create a calm haemodialysis unit that makes patients feel safe to undergo cannulation and survive its unpleasantness”. They further note that cannulation technique appears to influence whether patients feel safe in these settings as well—but that explorations into this phenomenon in their meta-analysis were limited, and additional research is now needed to elucidate how different cannulation techniques may impact pain and other measures of patients’ experiences in cannulation for haemodialysis.