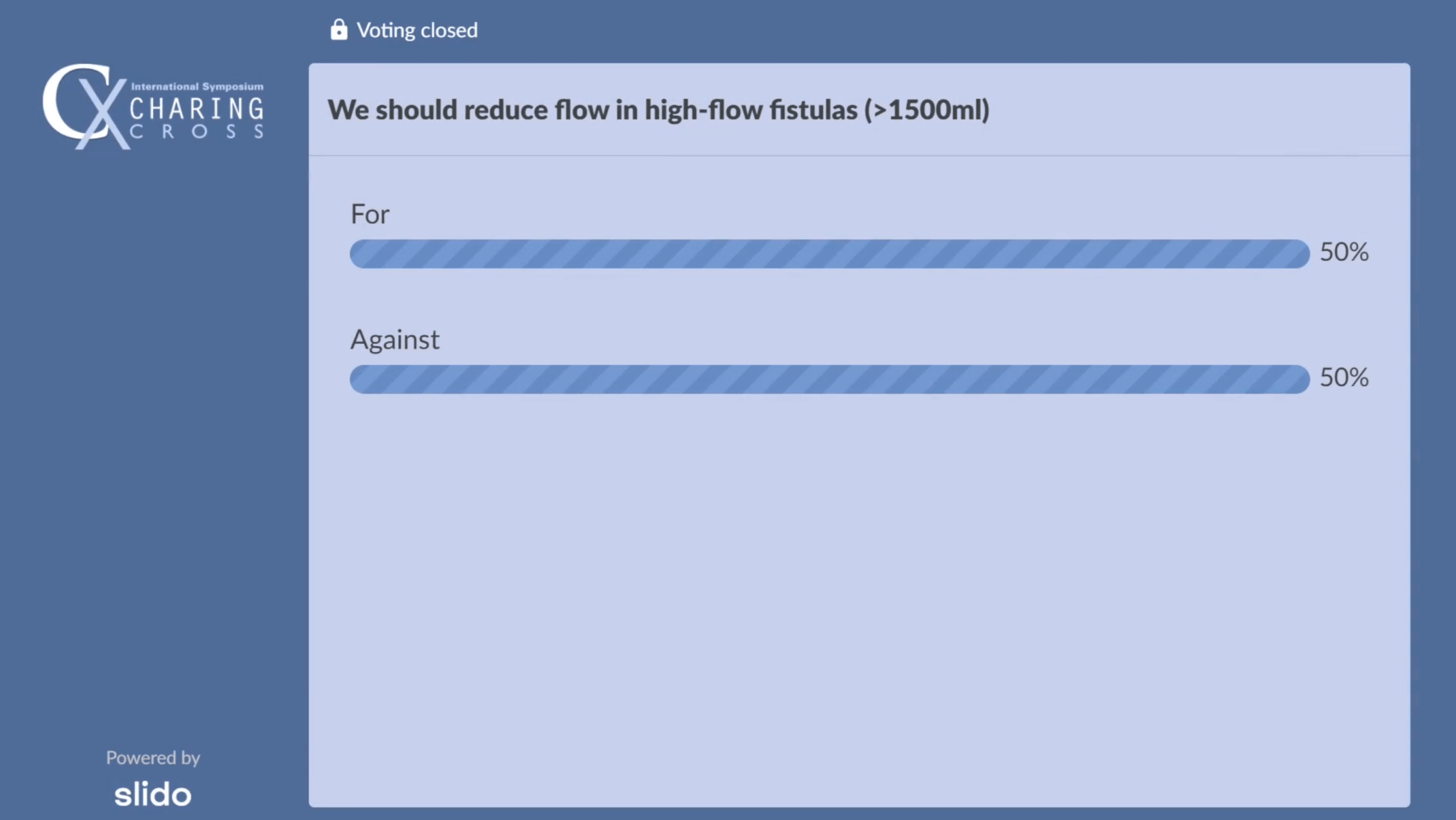
Discussions at this year’s Charing Cross (CX) 2021 Digital Edition (19–22 April, online) indicated that high-flow arteriovenous (AV) fistulas remain one of the more divisive topics in the field of vascular access. This was most apparent in the outcome of a debate on whether reducing flow in asymptomatic high-flow fistula patients is necessary, with audience polling revealing an exact 50/50 split across CX attendees.
Discussions at this year’s Charing Cross (CX) 2021 Digital Edition (19–22 April, online) indicated that high-flow arteriovenous (AV) fistulas remain one of the more divisive topics in the field of vascular access. This was most apparent in the outcome of a debate on whether reducing flow in asymptomatic high-flow fistula patients is necessary, with audience polling revealing an exact 50/50 split across CX attendees.
In the debate, the audience heard that high-flow fistulas can lead to major cardiac consequences and existing evidence demonstrates the prevalence of heart disease in renal patients, which begs the question: should flow be reduced in asymptomatic high-flow fistulas, or in transplant recipients, to prevent cardiac complications?
Renal and transplant surgeon Paul Gibbs (Queen Alexandra Hospital, Portsmouth, UK) argued in favour of the statement that ‘We should reduce flow in high-flow fistulas (>1,500ml)’. These points—and the debate motion more generally—were contested by transplant surgeon Surendra Shenoy (Washington University School of Medicine, St Louis, USA), who argued against the need for routine flow reduction in asymptomatic patients. Shenoy described the fistula as the “bystander” in these patients, adding: “Why shoot the fistula, which is serving them to stay alive?”
The hour-long session on high flow in access controversies, which was moderated by CX Executive Board members Nicholas Inston (Queen Elizabeth Hospital Birmingham, Birmingham, UK) and Domenico Valenti (King’s College London, London, UK), got underway with a presentation from interventional nephrologist Theodore Saad (Christiana Care Health System, Newark, USA). Saad introduced the audience to many of the existing challenges surrounding high-flow fistulas—including the fact that they often go “under the radar” due to complacency following fistula creation, as well as a lack of clear standards and uncertainties over which specialists should be responsible for them.
Saad also alluded to the connection between high-flow fistulas and cardiovascular problems, in addition to suggesting a more defined algorithm for managing and reducing flow in these structures is necessary—something he claimed he is currently working to develop and gain validation for. Inston concurred with many of Saad’s points, asserting that “the majority of renal patients die from cardiovascular causes” and “we should perhaps be designing some patient-related outcomes that measure this more effectively”, as well as asking about a point raised by vascular and renal transplant surgeon David Kingsmore (NHS Greater Glasgow and Clyde, Glasgow, UK) that a racing heart could be seen to be driving the fistula, rather than the other way around. Saad agreed on both counts, but did also respond to Kingsmore’s suggestion that the heart itself may be driving the fistula in these patients, stating that the two are “obviously interrelated” and separating them is not easy.
In the session following this, vascular and endovascular surgeon Robert Shahverdyan (Asklepios Klinik Barmbek, Hamburg, Germany) presented his initial clinical experiences using the Frame FR external stent (Vascular Graft Solutions). He described the device as an external banding tool used to support the vein at the anastomosis, adding that—having used the stent for high-flow arteriovenous fistula (AVF) repair in 43 patients—he believes it offers an additional, feasible and effective treatment for aneurysm and flow reduction. “It prevents redilation of the vein and further aneurysm formation, which also prevents recurrent high flow,” Shahverdyan commented.
Responding to a query from Valenti on the high proportion of cases with aneurysmal AVF in his patient cohort, which was 40 (93%), Shahverdyan stated: “The thing is, as our previous speaker said, how many patients actually get a follow-up to see if their fistula is high-flow or not? In the group I presented, four were kidney transplant patients and the rest were on active dialysis, and these patients come to ask if they can abandon their fistula. I would usually recommend reducing the flow instead of abandonment though. I know it is a controversial discussion over whether you should keep it or ligate it in kidney transplant patients—but I would reduce the flow and keep it in case the kidney transplant fails in the future”.
When asked by Inston what they considered to be the current “gold standard” for flow reduction procedures, Shahverdyan and fellow vascular surgeon Gaspar Mestres (Hospital Clínic de Barcelona, Barcelona, Spain)—who presented his views on the relationship between high-flow fistulas and steal syndrome during the session—both conceded they were unsure that one even exists right now. Following this, Saad brought the discussion to a close by suggesting that patient-led outcomes, such as pulse oximetry or pain, may be the most appropriate comparator in future studies to assess newer technologies for reducing high flow, a statement that drew a strong endorsement from Valenti.

Nephrologist Joris Rotmans (Leiden University Medical Center, Leiden, The Netherlands) followed this discussion with a presentation on the “chronic increase” an already-vulnerable patient’s cardiac output goes through as a result of vascular access creation for haemodialysis. This provided a fitting precursor to the CX debate on the question of reducing flow in high-flow fistulas, as Rotmans stated that while AVFs and AV grafts alike can increase the risk of left ventricular hypertrophy (LVH) and pulmonary hypertension, “the negative effects of an AVF on the heart can be reversed by an AVF ligation”.
He also concluded that it is currently unclear whether cardiac events and related mortality can be prevented through a greater emphasis on treating high-flow fistulas, but, when questioned by Valenti on certain instances of acute death after abrupt fistula ligation, Rotmans also theorised that a medical device capable of closing a functional fistula gradually—over the course of one or several days, for example—may be useful in offsetting these potential risks.
The ultimately contentious debate that followed this saw Gibbs argue in favour of reducing high flow first. His argument centred around the notion that “there is already evidence out there that high-flow AVFs are bad for our patients, and we do not need large, randomised trials to prove it”, and he cited multiple reports indicating that banding or revision using distal inflow (RUDI) procedures to reduce flow in AVFs can improve heart failure symptoms. Gibbs went on to argue that the absence of randomised controlled trials (RCTs) assessing the link between high-flow fistulas and cardiovascular complications should not detract from other evidence that the two are causally linked, pointing to the fact that there have been no RCTs to investigate the commonly-known, health-related consequences of smoking either.
In his counter argument, Shenoy emphasised many of the lines that have been drawn between high flow and cardiac symptoms to date are merely examples of association, rather than direct correlation or causation. He further claimed that existing studies indicating a trend between the two have either failed to properly compare dialysis patients with an AVF to regular, non-AVF dialysis patients, or have included many patients with underlying risks or prior history of cardiovascular conditions like congestive heart failure (CHF). Shenoy concluded his presentation by stating that, based on the currently-available data, “there is no role for routine flow reduction” in AVFs with a flow greater than 1,500ml per minute—but that closer monitoring and early intervention in these patients may be an optimal, alternative strategy.
The precedent for this being a particularly challenging, equivocal debate was set almost immediately by Inston following Gibbs’ and Shenoy’s presentations, as he conceded that he was “still undecided” on the need to reduce high flow. Gibbs added to this by stating that “we may be looking for the impossible study” when it comes to resolving the issue, although he also asserted that high-flow fistulas are “unnecessary”, and claimed: “If I had a fistula, I would want it running as low as possible in order to look after my heart long term”.
Rotmans, who had stated earlier that he feels “we should act far more aggressively than we currently are” to reduce high flow, also weighed in on the debate, arguing that preventative interventions similar to those used to treat cardiovascular disease should be deployed to reduce the fistula’s “obvious detrimental effects”. Shenoy countered this by reiterating his point that many regular haemodialysis patients experience similar cardiac symptoms to those who undergo AVF creation and, as such, there is “no direct proof” linking them.
In the discussion, Gibbs and Shenoy did agree on the need to treat patients with high-flow fistulas who are presenting with symptoms, but remained split on asymptomatic cases—as did the audience in attendance, with 50% voting for the motion, and 50% voting against, in a poll conducted at the end of the hour-long session.
The full session on high-flow fistulas in access controversies from the second day of CX 2021 can be viewed online here by registrants.