 The field of vascular access care for haemodialysis patients may look very different in just a few years’ time, with a host of new, innovative technologies currently being developed and tested to help tackle existing challenges relating to infection, the long-term patency of blood vessels, and complications arising from poor needle cannulation. Following a session from this year’s Vascular Access Society of the Americas 2021 Spring Virtual Conference (VASA, 21–22 May, online)—which saw nitric oxide (NO)-releasing devices, state-of-the-art optic sensors and bioengineered “living” arteriovenous (AV) grafts presented to the audience—various panellists, including engineers and clinicians alike, agreed that personalised, patient-centric approaches will be required to maximise the potential of these novel technologies in vascular access care as well.
The field of vascular access care for haemodialysis patients may look very different in just a few years’ time, with a host of new, innovative technologies currently being developed and tested to help tackle existing challenges relating to infection, the long-term patency of blood vessels, and complications arising from poor needle cannulation. Following a session from this year’s Vascular Access Society of the Americas 2021 Spring Virtual Conference (VASA, 21–22 May, online)—which saw nitric oxide (NO)-releasing devices, state-of-the-art optic sensors and bioengineered “living” arteriovenous (AV) grafts presented to the audience—various panellists, including engineers and clinicians alike, agreed that personalised, patient-centric approaches will be required to maximise the potential of these novel technologies in vascular access care as well.
Interventional nephrologist Karthik Ramani (University of Michigan, Ann Arbor, USA) kicked off the VASA 2021 session, entitled ‘What will vascular access care look like in 2025?’, by presenting a new approach to infection control for haemodialysis catheters: NO rechargeable fillers. Haemodialysis catheters, he claimed, are associated with “a great deal of morbidity and mortality, as well as a tremendous cost to the healthcare system”, with these issues often stemming from either catheter-related bloodstream infection, or inflammation whereby platelet activation leads to thrombosis in the blood vessel.
The solution Ramani presented is NitriCap (NitriCap Medical)—a single-use, antimicrobial catheter insert device that provides “superior protection” from bloodstream infections via the timed, controlled release of NO. As well as stating that NitriCap “overcomes many shortcomings of antibiotics in treating catheter-related bacteraemia”, Ramani outlined two in vivo real-world studies involving sheep that have assessed NitriCap versus a competitor product—ClearGuard HD (ICU Medical), which uses a different antimicrobial called chlorhexidine to reduce infections—and a standard haemodialysis catheter cap. He reported a 10,000-fold reduction in colony-forming units (CFUs) associated with NitriCap in both studies, and “superior antimicrobial efficacy” in all four regions of the catheter compared to both the standard cap and the competitor product.
In addition to the initial target area of tunnelled haemodialysis catheters, Ramani claimed that NO could subsequently be used in other spaces including temporary haemodialysis, peritoneal dialysis, and central venous catheters (CVCs), in the future, closing his presentation by quipping that “the future is definitely NOw”.
Moving from infection to another of the key unresolved issues in vascular access care highlighted by Ramani, namely chronic inflammation, a later presentation saw bioengineer Buddy Ratner (University of Washington, Seattle, USA) exhibit a novel method for reducing the formation of fibrosis that is often observed in synthetic vascular grafts following implantation—something that ultimately reduces graft compliance and long-term functionality. This contributes to dialysis access grafts having a 50% failure rate at one year, and therefore requiring routine maintenance, he added.
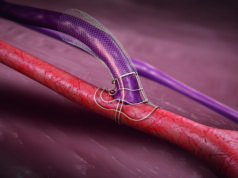
Ratner’s answer to this is a patented, bioengineered material dubbed ‘6S’, which holds the capacity to mitigate the foreign body reaction to an implanted graft. Its precision-porous structure reduces aggressive inflammation thus allowing the ingrowth of blood vessels to create an endothelium at the surface. The material has been used by Ratner and his colleagues at the Center for Dialysis Innovation (CDI) to develop a vascular prosthesis. Comparisons between this 6S prosthesis and a standard polytetrafluoroethylene (PTFE) graft in a sheep model resulted in the former looking like a “living artery” that was “pulsating nicely” when opened up at one month, according to Ratner, while a dense fibrotic capsule formed around the latter.
He concluded that, regarding the histology observed in these tests and others, “this is all looking very promising for a new mode of healing for synthetic grafts”, adding that the 6S biomaterial not only addresses inflammation, but also issues surrounding long-term durability, costs and regulatory hurdles that have plagued existing graft products for several decades. Ratner added that the 6S graft is now being examined further in sheep and pig models.
On a similar note, biomedical engineer Aijun Wang (University of California, Davis, USA) presented his own efforts as part of VasoBio—a company spun out of UC Davis and co-founded by Wang himself—to engineer a self-renewable, “living” surface for vascular grafts, improving their in situ endothelialisation and, ultimately, their long-term patency when used for haemodialysis. To this end, the ‘LXW7’ ligand, which holds a high affinity and specificity for endothelial progenitor cells and endothelial cells, was developed.
Wang asserted that, when compared to an untreated vascular graft surface, “we can see that—with the LXW7 coating, and cultured endothelial cells on top of it—the ligand can significantly increase the coverage of endothelium on the surface within three days”. He added that LXW7 was observed to have improved graft patency during a carotid artery bypass in a rat model and that, when progressed into a larger pig model, the luminal surface of a graft treated with the ligand was free from blood clotting, and had a smoother surface compared to an untreated graft at four weeks post implantation. Wang concluded that “this bioengineered approach can significantly improve the behaviour of these artificial vessels, and holds the potential for clinical use”.
Another presentation saw David Kuraguntla (San Francisco, USA), founder and CEO of Alio, discuss the need to combat the “significant healthcare burden” of kidney failure. Kuraguntla suggested bringing remote monitoring to the field of vascular access care may be the answer, presenting the results of a study assessing his company’s SmartPatch product—a wearable, 24/7 monitoring device that uses state-of-the-art optical sensor technology to measure volumetric flow rate, percentage stenosis and haemoglobin levels. Raw data from the SmartPatch is then processed in the cloud and analysed using machine learning, subsequently presenting these well-known, clinically actionable biometrics to a physician.
The study involved 128 haemodialysis patients across three centres, all of whom wore the device over their AV fistula—either in their upper or lower arm—for one week. According to Kuraguntla, the SmartPatch system measured haemoglobin with comparable or better accuracy and precision compared to available methods, detected low flow rates with 100% sensitivity and 75% specificity, and showed zero false positives and 100% sensitivity in detecting haemodynamically significant stenosis (>50%). In addition to concluding the study therefore demonstrates the SmartPatch’s round-the-clock monitoring capabilities, Kuraguntla concluded that, more generally, “remote monitoring systems show potential promise in improving the care and lowering the costs associated with dialysis access”. He also stated a belief that increases in home dialysis and value-based models have enhanced the need for these types of integrated, remote monitoring solutions even further.
Bioengineer Joseph Singapogu (Clemson University, Clemson, USA) closed the session by presenting his attempts to tackle the various issues stemming from poor needle cannulation—including vascular access complications, increased reliance on tunnelled dialysis catheters, and the anxiety and pain it can cause patients. He asserted that there is a direct link between cannulation outcomes and the skill of the clinician who is cannulating, but, despite this, cannulation training today is limited and relies on “antiquated tools”.
Singapogu claimed that simulators, which have already been adopted in other medical specialties like minimally invasive surgical procedures, could help to improve this state of affairs, citing the fact that they allow for safer practice that takes place in a non-clinical setting, create objective metrics for assessing skill levels, and can even provide personalised feedback to improve these skill levels. As such, he presented the “first ever” state-of-the-art simulator for haemodialysis cannulation, which consists of a layer of artificial skin and a range of sensors to measure several parameters including pinch forces, needle motion and angle, the time taken to cannulate, and even palpation technique prior to inserting the needle.
Singapogu said the main goal behind his novel simulator is to provide a standardised way of measuring cannulation skill, whereby “subjectivity is minimised” because the approach is heavily metrics driven. “I believe the future of cannulation skills training will be simulator-based”, he added, also claiming that, despite being a work in progress, his technology has the potential to deliver personalised feedback and make cannulation training safer. “Currently, our simulator is quite expensive, but we do hope to have a lite version in the future that could be used in area clinics,” he concluded.
Challenges and priorities ahead for vascular access innovations
A discussion following this session on the future of vascular access care saw one of the moderators, nephrologist and co-director at UNC Kidney Center Prabir Roy-Chaudhury (University of North Carolina, Chapel Hill, USA), reflect that “there was clear evidence that—if we want to move the needle—there has to be cooperation and collaboration between engineering and medicine” before posing a question to the panel over what would be more suitable: a one-size-fits-all approach to vascular access technologies, or a pathway of individualisation, whereby specific patient populations are identified and targeted.
The consensus among the panel was that the latter will be more appropriate moving forward, with Ramani stating that he hopes NitriCap and other technologies presented at VASA 2021 will serve a large population—but that, ultimately, “we still have to personalise our care” and it will “definitely not be a one-size-fits-all approach”. On a similar note, Ratner added that he and his colleagues at the CDI believe “patient feedback is absolutely critical to developing new products, and what we find is that one size does not fit all, because people want things customised to their own specific needs”.
The discussion’s other moderator, vascular and interventional radiologist Sanjay Misra (Mayo Clinic, Rochester, USA), then moved the subject on to where animal models—which were used, and continue to be used, to assess several of the technologies on show in the earlier session—fit into product testing. Regarding the bioengineered grafts specifically, he said: “One challenge of animal models is the endothelialisation differences among species, and getting trapped with observations in just one species may prove to be a problem.” Misra added that this presents a challenge that the US Food and Drug Administration (FDA) has to deal with by helping investigators understand the biology of what they are testing their products on.
Wang weighed in on this topic by stating that all three of the species his LXW7 ligand has been tested in so far—rats, pigs and sheep—are all widely used in existing literature in this space, also asserting that, at UC Davis, they have seen “pretty consistent results in terms of binding and in vivo functional analysis”. Vascular and endovascular surgeon Jeffrey Lawson (Duke University, Durham, USA), who is also the immediate past president of VASA, added to this by stating that endothelialisation of vascular conduits in animal models is “more complicated than we would like, because certain animals tend to repopulate synthetic conduits in ways that are very different to what we see in humans”—something that he claimed is “accepted within the legacy of studying vascular materials”. Ratner concluded that there is “a huge disconnect” that needs to be addressed between results for synthetic grafts in humans and animals, and that “animal models are not giving us the information we need” when it comes to endothelialisation.
Another potentially more distant challenge that these types of novel technologies may face was also highlighted by Misra—that being access to fundraising, as well as the fact that “getting these technologies into humans is the ultimate goal…but it becomes very expensive, very fast” to conduct first-in-man clinical trials. In response, Ratner agreed that funding is a “critical issue”, noting that partnerships with industry have been “very useful” in his experience of developing new products, while Wang added that collaboration with clinicians and researchers can also play an important role, in his view.
Regarding regulatory burdens, which was another issue raised by Misra in the discussion, Ratner referred to previous instances of struggling to secure funding from the FDA due to a lack of available preliminary data, and stated: “We have had a few philanthropic gifts that have been very helpful, but I am just a little bit disappointed in our national funding agencies for their inability to take these things all the way, in a translational sense.” Misra responded by stating that, in his experiences with the FDA and the US National Institutes of Health (NIH), one “really big problem” that exists in innovation is that “the funding priorities are not in line with the unmet clinical need” for vascular access innovations.
While he did agree with the other panellists on the importance of philanthropy and angel investors, as well as venture capital (VC) and non-typical federal funding, Roy-Chaudhury opted to end this part of the discussion on a positive note by stating that “through organisations like the Kidney Health Initiative, there is now more partnership with the FDA—who have been huge supporters of many of the things we have been speaking about”. In closing the session, he added: “I hope that things are changing with more awareness in federal agencies, and in the community as a whole.”