As a part of the Novel technologies in haemodialysis access session on the final day of the 2024 VEITHsymposium (19–23 November, New York, USA), Ellen Dillavou (WakeMed Heart Center, Raleigh, USA), primary investigator (PI) for the VenoStent trial, presented new data about the SelfWrap (VenoStent) bioabsorbable perivascular wrap, outlining how the novel device can, in her words, improve arteriovenous fistula (AVF) maturation and patency.
Beginning her presentation, Dillavou outlined the problem that the device aimed to solve; according to data published in the Journal of the American Society of Nephrology (JASN) and in American Journal of Kidney Disease (AJKD), annually, five million patient lives are put at risk by 60% one-year failure rates of AVFs and arteriovenous grafts (AVGs), as well as 20% one-year failure rates of vein grafts in bypass grafting. She also highlighted that these one-year failure rates were resulting in US$3 billion in direct costs to the Centers for Medicare & Medicaid Services (CMS).
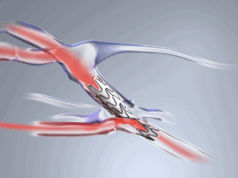
One solution for these issues, Dillavou argued, is the SelfWrap device. Receiving its US Food and Drug Administration (FDA) breakthrough device designation in May 2022, followed by investigational device exemption (IDE) approval in May 2023, this vascular wrap made of bioabsorbable polymers uses an artery-like mechanical support to help veins first “behave” and then “become” like an artery. It also regulates flow—which Dillavou stated will “impart haemodynamic benefits” such as reduced turbulence—and promotes both the outward migration of vascular smooth muscle cells and downstream expansion.

Another benefit of SelfWrap, according to Dillavou, is that it is able to circumvent the primary outcome contributing to a failure rate of over 50% in vascular surgery: neointimal hyperplasia (NH). “In every large animal model which tested AVFs, AVGs, and bypass grafts over five years and three different centres, the advanced materials approach that ‘arterialises’ veins significantly reduces NH,” said Dillivou.
The presentation then proceeded to examine the design of the study. The trial’s objective was to demonstrate feasibility and evaluate the safety and performance of the SelfWrap device by enrolling 20 participants in a single-centre, prospective, single-arm study, with follow-up obtained at six months up to 60 months. The primary endpoint was a high patency rate.
For the 20 patients that were enrolled, three SelfWrap sizes were employed, with selection based on vein size. A total of 13 patents (65%) were given brachiocephalic fistulas (BCFs), two received basilic vein transpositions (BVTs), and five were given radiocephalic fistulas (RCFs).
One aspect of the study that Dillavou highlighted in particular was that, based on the Lok Criteria— a method for predicting AVF maturation failure based on race, elderly status, peripheral arterial disease (PAD), and carotid artery disease (CAD) status—20 patients were high-risk in the trial population, with the criteria predicting that >42% of subjects in the study would fail to mature. “This doesn’t take into account the presence of more female than male patients”, Dillavou noted, “all of whom had ESRD [end-stage renal disease], were on haemodialysis, and had smaller than average vessel sizes.”
Moving on to the results of the study, Dillavou reported that there were no adverse events probably or definitely related to the device through 36 months, as well as no device deficiencies nor adverse device effects.
Looking at the primary endpoint of the study, the VEITHsymposium audience was told that the SelfWrap device had a high maturation rate; functional maturation (defined as two-needle cannulation for more than 75% of dialysis sessions within four consecutive weeks) was 95%, compared to the <58% expected maturation rate, and unassisted maturation (defined as two-needle cannulation without requiring an intervention [excluding superficialisation and one collateral ligation] to do so) was 90% for SelfWrap, compared to 33% for the benchmark.
The device also had a high catheter removal rate; SelfWrap saw 89.5% of catheters removed at nine months, 94% of which were unassisted, compared to ~27% at nine months for untreated AVFs in a Clarke et al publication. The study also saw a low rate of interventions for patients receiving the SelfWrap device. According to Dillavou, there have been four total interventions to date, two of which were on premature AVFs: three were percutaneous transluminal angioplasty (PTA) for juxta/anastomotic stenosis, and one was surgical revision and stent placement for upper arm cephalic vein stenosis. Through 36 month follow ups, the rate of interventions per patient year (PPY) was 0.12, compared to 1.9 interventions PPY for standard of care.
Bringing her presentation to a close, Dillavou noted that, should these results be translated to the ongoing IDE study, “these results would be very impactful for chronic kidney disease/ESRD patients requiring haemodialysis”.