Failure of home haemodialysis (HHD) treatment, defined as a return to in-centre haemodialysis (ICHD), has been associated with a “significant increase” in mortality when compared to continued HHD—a trend that was observed in both the early (first 30 days and 30–90 days) and late (>90 days) periods following treatment failure. This is according to data published in the American Journal of Kidney Diseases (AJKD).
In reporting their results, lead author David J Semple (Department of Renal Medicine, Auckland District Health Board, Auckland, New Zealand) and colleagues also note: “Competing risk analysis showed that withdrawal from dialysis, but not cardiovascular death, was a significant cause of early (<90 days) death after return to ICHD from HHD. However, from 90 days onwards, withdrawal from dialysis and cardiovascular death were both significant causes of death.
“In this study, we wanted to understand what happens after a person moves from HHD to ICHD by comparing the rate of death as patients moved between treatments,” they continue. “We found that the risk of death is high following the transition and remains high after three months. We could not discern the cause of this association, but suspect it is due to the events that caused patients to stop HHD. The group of patients who stopped haemodialysis only for a period of time did not have an elevated rate of death—we suspect this is because they did not transiently stop HHD due to serious illness.”
The researchers’ retrospective, multicentre, large-scale cohort study included all patients represented in the Australia and New Zealand Dialysis and Transplant (ANZDATA) registry who commenced haemodialysis between 2005 and 2015, and were treated for more than 90 days. The primary outcome of the study was all-cause mortality. Semple et al add that patients were followed from the date of initiating haemodialysis to death, transplantation, transfer to peritoneal dialysis, loss to follow-up, or the study’s end in December 2015.
Between January 2005 and then, a total of 23,358 patients commenced haemodialysis in Australia and New Zealand, of which 19,306 (82.7%) remained alive on haemodialysis for more than 90 days. Some 2,554 patients (13%) received HHD at any point during the study period. Median follow-up time was 2.2 years, mean age at dialysis start was 60.8 years, 62.1% of the patients were male and almost 49% had diabetes.
During follow-up, 6,972 patients died—a crude rate of 13.6 per 100 patient years. The authors note that the crude death rate was highest in ICHD patients with no prior HHD (14.9 per 100 patient years) and ICHD patients with prior HHD (14.4 per 100 patient years), and lowest in patients in their first HHD episode (4.4 per 100 patient years) and patients with HHD, and prior ICHD and HHD (5.9 per 100 patient years).
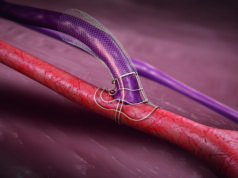
They add that the mortality rate in ICHD patients with prior HHD was 20.6 per 100 patient years during the first 30 days, 17.5 per 100 patient years at 30–90 days, and 13.6 per 100 patient years beyond 90 days, meaning that—across all three of these timeframes—univariate and multivariate analysis showed a transition from HHD to ICHD (HHD treatment failure) was associated with an increased risk of death. Other significant independent covariates for death included patient age, late referral, smoking status, cause of end-stage renal disease (ESRD), and the presence of major comorbidities, including coronary artery disease (CAD), chronic lung disease and diabetes. Non-Caucasian ethnicity and the use of an arteriovenous fistula for dialysis access were associated with a reduced risk of death. However, of these covariates, only patient age was associated with a “similar magnitude” of risk for mortality to HHD treatment failure.
Withdrawal from treatment (n=2,500, 4.9 per 100 patient years) and cardiovascular events (n=2,246, 4.4 per 100 patient years) were the most common causes of death, the study found, while infection (n=631, 1.2 per 100 patient years), malignancy (n=386, 0.8 per 100 patient years) and “other” (n=1,212, 2.4 per 100 patient years) were less frequent causes of mortality.
“In common with other observational and registry studies, the HHD patient state was characterised by favourable demographic and clinical characteristics, and a significant survival advantage of HHD over ICHD was demonstrated,” Semple and colleagues write. “Other studies have explored how much of this relates to the benefits of HHD over ICHD, and how much relates to residual confounding of the highly selective patient group entering HHD. However, in this study, significant residual confounding likely remains between those starting HHD and those never exposed to the treatment modality—due to the lack of data on patient socioeconomic status.”
The authors also note that their “key novel finding” of HHD treatment failure being associated with a significantly increased risk of early and late death may be “less vulnerable to the residual confounding inherent in a registry study of this type”, due to all patients restarting ICHD after a period of HHD having, at one stage, the clinical and socioeconomic attributes enabling a successful initiation of HHD. They add that, as such, it “represents an important finding that should stimulate additional investigation” into the causes and implications of dialysis modality changes.
“No conclusions on the underlying mechanism for this increased risk of death after HHD treatment failure can be drawn from this study,” Semple et al conclude. “The causes of HHD treatment failure were not available for investigation in this dataset, but clinical experience tells us that the transition from HHD to ICHD most often represents a regressive step in a person’s dialysis career—often triggered by adverse health events—and it is likely this, rather than the change from HHD to ICHD, that is responsible for the increased risk.”