A single-centre, retrospective, comparative study, which was presented at the July 2021 Journal of Vascular Surgery (JVS) Journal Club (14 July, online), has found that percutaneous arteriovenous fistula (pAVF) creation may be associated with lower rates of complication relating to wound healing or infection, and a lower rate of surgical reinterventions at long-term follow-up, compared to surgical AVF (sAVF) creation.
A single-centre, retrospective, comparative study, which was presented at the July 2021 Journal of Vascular Surgery (JVS) Journal Club (14 July, online), has found that percutaneous arteriovenous fistula (pAVF) creation may be associated with lower rates of complication relating to wound healing or infection, and a lower rate of surgical reinterventions at long-term follow-up, compared to surgical AVF (sAVF) creation.
Matthew Smeds, professor of surgery in the Division of Vascular and Endovascular Surgery at St Louis University in St Louis, USA, began the online session by outlining the key potential benefits associated with pAVF creation—those being that they avoid surgical scarring, minimise vessel trauma while creating consistently-sized connections, often achieve dual outflow, and result in lower flow rates, which may diminish complications caused by intimal hyperplasia and other outflow-related issues.
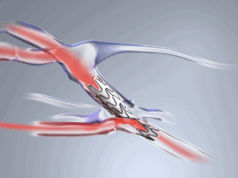
He also noted that the WavelinQ endoAVF (BD) and Ellipsys vascular access (Avenu Medical/Medtronic) systems are the two “main players” in this space right now. However, while there is a strong body of literature on both of these devices and their benefits—including data suggesting they boast high cannulation success rates and low reintervention rates—Smeds stated that there are very few existing articles that provide a direct comparison to sAVF.
Following this, he handed over to Charles Marquardt, an integrated vascular surgery resident at St Louis University, to discuss a study entitled “Comparison of surgical versus percutaneously created arteriovenous hemodialysis fistulas”, which is published in JVS by Ghazi Harika (Groupe Hospitalier Paris Saint-Joseph, Paris, France) et al.
The study was conducted retrospectively over 12 months, and sought to compare pAVF creation with the Ellipsys system to sAVF creation. Maturation, and primary and secondary patency, were the primary outcomes of the study, with secondary outcomes being numbers and types of reinterventions, and complications, including wound healing, infection and steal syndrome.
Regarding the results, Marquardt reported that the characteristics between the pAVF (107 patients, average age=63.6 years, 38.3% female) and sAVF (107 patients, average age=63.5 years, 39.2% female) groups were “generally similar”, although more patients in the pAVF group (60.7%) were already on haemodialysis at the time they underwent access creation compared to in the sAVF group (46.7%).
He also noted that rates of maturation at six weeks were higher in the pAVF group (65% compared to 50%), but that primary patency rates at 12 months were higher in the sAVF patients (86% compared to 61%). Wound infection rates at 12 months were found to be lower in the pAVF group (0.9% compared to 9%) and, while reintervention rates were lower in the sAVF group after 12 months (36% compared to 53%), this shifted at 24 months, with the rate of surgical interventions being lower in the pAVF group (17% compared to 36%) and the rate of percutaneous interventions being similar. Patency rates and the rate of other complications were similar between the two groups at the two-year follow-up.
“In the paper, primary patency is highlighted as being much higher in the sAVF group, while the pAVFs that were created were quite small, at about 4mm, and required an angioplasty,” said Marquardt. “But, once that angioplasty had occurred, they matured well and did not require much in the way of secondary intervention—and that is why there is an evening out of the numbers between the two groups. The secondary patency at about 300 days equalised between the two groups as well.”
Marquardt concluded that, in terms of secondary outcomes, wound infections and surgical reinterventions were “much lower in the percutaneous group—as would be imagined”, before stating that another advantage of pAVF creation is that it can be performed by a wider range of physicians, including vascular surgeons, interventional nephrologists and interventional cardiologists. He also noted, however, that limitations of the study include its retrospective nature, the risk of patient selection bias, and a lack of data on the size of the vessels in each group.