New technologies intended to improve the often-mixed outcomes associated with arteriovenous grafts (AVGs) for haemodialysis access were on display at this year’s Vascular Access Society of Britain & Ireland scientific meeting (VASBI; 16–17 September 2021, virtual). In addition to insight on the Wrapsody endoprosthesis (Merit Medical Systems) from James Gilbert (Oxford University Hospitals NHS Foundation Trust, Oxford, UK), two other innovative grafts—each designed to tackle unique, unresolved problems in this space—featured prominently.
The session, entitled “Updates and Developments in Dialysis Access”, first saw Jeffrey Lawson, adjunct professor of surgery at Duke University Medical Center (Durham, USA) and chief surgical officer at Humacyte, present attendees with the human acellular vessel (HAV; Humacyte)—a bioengineered graft intended for use in haemodialysis access, as well as vascular trauma and peripheral arterial disease (PAD). He initially noted that synthetic graft products, often made from expanded polytetrafluoroethylene (ePTFE), are already in use in the USA due to high non-maturation rates associated with arteriovenous fistulas (AVFs), but that only about 70% of these remain functional as a dialysis access option at one year due to either infection or failure modes at the anastomosis.
Lawson claimed that the HAV, which is grown from human vascular smooth muscle cells, is usable within one month of implantation, and appears to be highly resistant to infection and has demonstrated long-term durability and limited intimal hyperplasia in ongoing clinical studies. Referencing results from a Phase II study of the HAV for haemodialysis access specifically, he reported improved six- and 12-month secondary patency rates compared to historical data on autologous fistulas and ePTFE grafts, in addition to reduced infection rates and positive safety outcomes.
Lawson claimed that the HAV has displayed an ability to repopulate and remodel itself with the patient’s own cells over time—a feat that has been achieved consistently, regardless of the host’s age—and has also been shown to not stimulate an immune response, with no reported instances of clinical graft rejection across more than 430 patients. Five-year results from end-stage renal disease (ESRD) patients implanted with the HAV in the Phase II study have been submitted for publication, he added, and two multicentre, Phase III studies are currently ongoing to directly compare the bioengineered graft to traditional AVFs and AVGs in haemodialysis access.
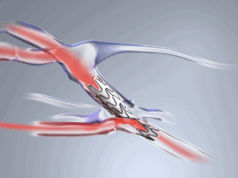
Later in the same session, Shawn Gage—an adjunct instructor for the Duke University Physician Associate Program (Durham, USA)—presented the InnAVasc graft to the VASBI audience. Gage, who is also InnAVasc founder and director of clinical operations, began by highlighting the many issues in dialysis access including haematoma, external bleeding, pseudoaneurysm and localised infection, that stem from problems with graft cannulation. He also pointed to a report published in the Journal of Vascular Access (JVA) that suggests that, across traditional AVGs and AVFs, needling complications may account for as much as 20% of all access-related complications.
Gage then discussed the InnAVasc graft in more detail—stating that it has been designed to prevent these needling complications with features such as cannulation pods and ridges that give the cannulator a very specific and identifiable site to puncture, a back plate that prevents the needle from puncturing the other side of the graft, and self-sealing materials that reduce or eliminate bleeding. In addition to noting that no needle-related complications or injuries have been observed in the graft across 42 patients and 5,500-plus cannulations, Gage claimed that cannulation complications are likely to be a bigger problem than is currently being recognised in dialysis access, with further research and improved materials being required to ameliorate this situation.
Gage went on to discuss how improved safety features like those seen in the InnAVasc graft could represent a major advantage for patients interested in transitioning to home haemodialysis and hold the potential to bring about a new generation of home therapies for kidney failure patients.