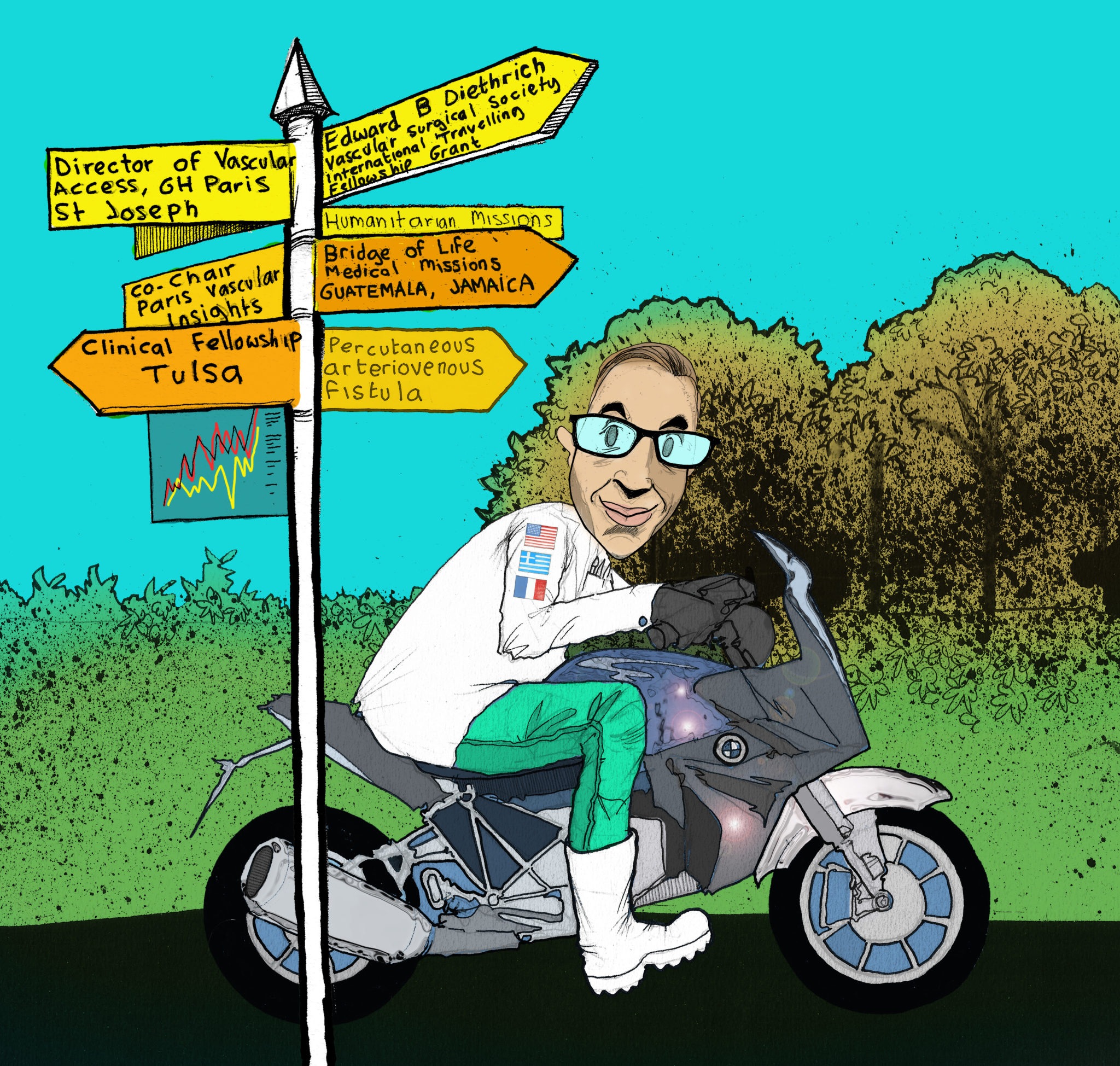
 Born and raised in the small lakeside city of Kastoria in northern Greece, Alexandros Mallios’ 15-year journey as a vascular surgeon has seen him complete a year of national service in the Greek military, travel to far-flung parts of the Caribbean and Central America to perform complex procedures, and work with a number of pioneering physicians in the field. Today, he is the director of the Vascular Access Center at Hôpital Paris Saint-Joseph in Paris, France and chief of vascular surgery at Centre Hospitalier de Chartres in Le Coudray, France. His achievements include pioneering and performing the first ever percutaneous arteriovenous fistula (pAVF) creation with the Ellipsys system (Medtronic) in Europe, and co-founding the Paris Vascular Insights (PVI) conference.
Born and raised in the small lakeside city of Kastoria in northern Greece, Alexandros Mallios’ 15-year journey as a vascular surgeon has seen him complete a year of national service in the Greek military, travel to far-flung parts of the Caribbean and Central America to perform complex procedures, and work with a number of pioneering physicians in the field. Today, he is the director of the Vascular Access Center at Hôpital Paris Saint-Joseph in Paris, France and chief of vascular surgery at Centre Hospitalier de Chartres in Le Coudray, France. His achievements include pioneering and performing the first ever percutaneous arteriovenous fistula (pAVF) creation with the Ellipsys system (Medtronic) in Europe, and co-founding the Paris Vascular Insights (PVI) conference.
What initially attracted you to medicine, and the field of vascular access in particular?
Believe it or not, I decided to study medicine because I was fascinated with human psychology and wanted to become a psychiatrist. In medical school, I got to observe some of the first endovascular stent grafts for abdominal aortic aneurysm (AAA) by one of their pioneers, Konstantinos Papazoglou—I am not sure if I was impressed by the nature of the interventions or by simply watching someone who is far better than his average colleagues, but it definitely impacted my decision to choose vascular surgery as a speciality. My interest in vascular access probably coincided with me working alongside Myriam Combes in Paris and, later, with William “Tip” Jennings in Tulsa.
Who have your mentors been and how have they impacted your career?
I was really blessed and lucky to meet and work with people like Roy Greenberg, Jean-Pierre Becquemin, Martin Malina, Thomas Fogarty and Edward Diethrich. These extremely gifted people can positively affect someone’s life with a simple word or piece of advice. I will never forget when, after a presentation I gave as a recipient of Edward Diethrich’s scholarship, he came to me and simply said: “Well done, I am proud of you.” It was one of the most important moments of my life. He was like a rockstar from another planet—not only as a doctor and surgeon, but as a person too. Besides these very special people, I developed a relationship of mentorship and friendship with three people: Konstantinos Papazoglou, Benoit Boura and Tip Jennings. They were all there for me in different moments of my life to support and advise me, and I will always remain particularly grateful.
What do you feel has been the most important development in the field of vascular access during your career?
Indisputably, the percutaneous creation of arteriovenous fistulas (AVFs) is the most important development in vascular access and one of the most important in vascular surgery too. It is transformational in ways that will become obvious 10–15 years from now. People will look back on pictures of huge aneurysmal fistulas and find it difficult to believe this was acceptable in medicine. It made vascular access surgeons think about anatomy and physiology in a totally different and unconventional way, and patient preferences for this new technology have meant there is little space for laggers to resist these changes.
EndoAVFs are a relatively new concept. How do the two main systems stack up against each other in terms of creation, and maintenance in the long term?
Both systems are similar as they create a communication in a location where a vein lies next to the artery, and then rely on the perforator to bring this blood up into the superficial system and enable its use for dialysis. However, they are different in terms of energy used and exact location. Ellipsys most likely needs better ultrasound skills for the puncture, while WavelinQ (BD) probably has different challenges as the connection is in a location that is a bit more variable and distant than the precious perforator vein. Both systems and the companies that have acquired them serve the promise for medical innovation and better patient care very well.
Besides your own work, what is the most interesting piece of vascular access research you have seen in the past year?
I think new data that came out from a recent randomised controlled trial in the New England Journal of Medicine (NEJM) on drug-coated balloons (DCBs) in vascular access are very promising, and they have relieved our anxiety about mortality issues and highlighted a potential for fewer interventions. Covered stents can also be promising in some locations in order to completely cover the diseased segments. While AVFs are preferred, we need to be aware that a diseased vein cannot provide a good-quality AVF, and we should not hesitate to use newer technologies if they can improve the patient’s quality of life and survival chances—which is essentially what we do when we provide reliable access for dialysis.

What is the most significant unmet need in the field right now?
I think the Achilles’ heel is still the fact multiple reinterventions are required for the majority of patients. We need to reach a point where we will be able to say to most patients that multiple reinterventions will be exceptional, and not the rule.
What are you seeking to achieve with the vascular access component of the Paris Vascular Insights meeting?
Together with Yann Gouëffic, Stéphan Haulon, and the other organisers of PVI, I would like to strengthen it and establish it as one of the top five, or even top three, vascular meetings in the world. This year, we have a new venue, and a total remake of the style and overall organisation of the event. The same goes for the access session—I want it to be one of the meetings that specialists from all over the world will not want to miss each year as an opportunity to learn and have fun together.
How did your period in military service influence you as a physician?
From the moment we enter medical school, we become fairly confined in terms of our social interactions and interests—all our friends are doctors and all of our discussions are around medicine. At the age of 31, I started my military service much older than the other cadets. I was very stressed, and worried about how I would cope with people giving me orders, but it ended up being one of the best and more relaxed periods of my life. I got to interact with soldiers from all possible backgrounds and cultures. I was like an older brother for the ones that were a bit more fragile and sensible. I made some good friends, and one great one—general Christos Drivas—who later became the godfather of my youngest daughter.
You have previously taken part in humanitarian missions in Jamaica and Guatemala. What were your experiences and takeaways from practising in these surgically austere environments?
Those mission trips are definitely a life-changing experience, and they provide a stress test for your technical and social skills. For one week, you are an “invited invader” of a local system, and you have to do the maximum amount of good and zero harm, if possible. While there are some excellent local colleagues that act as coordinators and make things easier—and patients and families are grateful for your service—the rest of the hospital, the rest of the country, even, are not necessarily fond of you being there. Access to resources and overall support is limited, there are many patients waiting on you as a messiah to perform their surgery, and there is also no one to fix complications after you leave. It is a very unique cocktail of factors!
What advice would you give to people embarking on a career in the field of vascular access?
The same advice I would give to anyone for any profession: make sure you love it and you are having fun when you are doing it. I am lucky because I am having fun in the operating room. No matter how tired I am when I operate, I am enjoying it, which makes everything much easier.
What are your interests outside of the field of medicine?
I love sailing and swimming with my daughters, and I will do this a lot more as they get older. I enjoy riding my motorcycle whenever I find time and the French weather allows. I also enjoy reading about politics and the global economy, and, although I am still a rookie, I do a bit of day trading—including lots of emotional trades that make me lose in five minutes what I have made in one week! It is very frustrating but there is a certain process of mastering yourself, and your actions and emotions, that I find to be a very interesting personal challenge. At this stage, I am still like a first-year resident with a scalpel in his hand—not very trustworthy. But, who knows, I may get good at it one day and be able to operate only for fun, during missions, and to train young surgeons.
Fact file
Current appointments:
- Vascular surgeon and director, Vascular Access Center, Hôpital Paris Saint-Joseph, Paris, France
- Chief of vascular surgery, Centre Hospitalier de Chartres, Le Coudray, France
Education:
- 2001: MD, Aristotle University, Thessaloniki, Greece
- 2003–06: General surgery resident, Thessaloniki, Greece
- 2007–08: Military service, Greece
- 2008–12: Vascular surgery resident, Paris, France
- 2012–14: Vascular surgery fellow, Tulsa, USA
Honours (selected):
- 2010: International Travelling Fellow Grant, Edward B Diethrich Vascular Surgical Society, Scottsdale, USA
- 2010: Best Poster Presentation, European Society for Vascular Surgery (ESVS) Annual Conference, Amsterdam, The Netherlands
- 2020: Pioneering pAVF creation efforts with Ellipsys system published in Journal of Vascular Surgery (JVS)
- Conference director, International Vascular Access Symposium and PVI, Paris, France












