Arteriovenous fistulas (AVFs) are widely considered to be the holy grail in dialysis access, providing a more long-term solution than synthetic arteriovenous grafts (AVGs) or central venous catheters (CVCs), with a reduced risk of complications. However, these benefits only come into play once the fistula has become functional—prior to this stage, they carry their own set of potential drawbacks with the risk of non-maturation, whereby the fistula is still not providing a suitable dialysis access option several weeks after surgery, chief among them. Joris Rotmans, chair of the Department of Nephrology at Leiden University Medical Center in Leiden, The Netherlands, and president-elect of the Vascular Access Society (VAS), discusses the reasons why AVFs achieve maturation so inconsistently and outlines ongoing efforts to solve this longstanding problem.
The problem of AVF non-maturation ultimately stems from the fact that a fistula is an artificial connection, which disturbs the natural homeostasis in a vein by instigating an excessively high rate of blood flow. “In general, [AVF creation] is unphysiological,” Rotmans states, “because we want the veins to do something that they are not designed to do.” He goes on to note that, while current European guidelines still lean towards a fistula-first approach to dialysis access, there has been a slight shift away from this within US guidance in recent years, in particular when it comes to elderly patients, due to the lengthy maturation period and potential secondary interventions associated with AVFs.
Various clinical studies have indicated that roughly 50% of patients need at least one subsequent intervention to make their fistula functional and, overall, about 75% of fistulas end up achieving maturation—a fact that, according to Rotmans, will frequently lead to patients choosing an AVG or CVC instead, especially in countries where shared decision-making is more prevalent across healthcare systems. “However, once you have a functional fistula, the complication rate is by far the lowest compared to other access options,” he continues. “It is the early phase where there are a lot of hurdles but, once it is up and running, everybody is convinced that it is the best option.”
Risk factors for non-maturation
“In terms of risk factors, female sex is the most important by far,” Rotmans notes. “Women have an almost two-fold increased risk of non-maturation, and that is consistent in numerous studies from all over the world.” He goes on to state that the underlying causes of this phenomenon have not yet been uncovered, with the initial theory attributing it to female patients having smaller blood vessels also being ruled out as an explanation by these studies. “In the current guidelines, in my opinion, female sex is not being recognised enough, because there is no differing policy with regard to selecting the optimal access in female patients compared to male patients—and, I think that, when you are anticipating the risk of non-maturation, the sex of the patient should be considered in the equation,” he adds.
While older age and previous cardiovascular disease have both been highlighted as potential risk factors for non-maturation in some studies—but not unequivocally proven to date—the previous use of CVCs, as well as other instances of needling in the blood vessels themselves prior to fistula creation, are more well-established as being associated with a heightened risk of non-maturation, with “feed preservation” therefore being encouraged in the lead up to a patient beginning dialysis. Rotmans notes that the access surgeon’s level of experience is important in fistula outcomes as well—but is arguably the most challenging factor to quantify with data.
Multifaceted approach needed?
The possibility of directly aiding AVF maturation is still an area shrouded in uncertainty. Previously, animal models and preclinical studies have indicated that elastin plays a notable role in fistula maturation. However, subsequent clinical trials showed no substantial benefit to modifying the levels of this protein in the vessel walls of patients. Similarly, Rotmans says, there was previously a belief that inhibiting the overall inflammatory response caused by AVF creation may improve maturation rates—but, once again, clinical trials involving liposomal prednisolone for this purpose yielded disappointing results.
Rotmans goes on to state that translating the role played by these specific proteins and factors into clinical benefits is challenging because there are numerous interlinked processes involved in fistula maturation. “There are hundreds of genes involved here and modulating one of them is not going to make a difference for patients in the future, in my opinion,” he adds, claiming that, because of this, a combination therapy may be required to change this uncertain outlook. “You really need to influence multiple pathways to steer the vessel in the right direction,” he says. “So, I am convinced that the local administration of drugs—during surgery, or by clever labelling to guide them to the vascular access site—is the way to influence maturation.”
A dynamic solution
Tackling the problem of fistula maturation at the source is another approach that is currently being investigated, according to Rotmans. More specifically, reducing the consistently high rate of blood flow through the anastomosis—which is a “substantial part” of the problem of non-maturation and also plays a role in long-term fistula failure—has been explored, with creation above the elbow or in the upper arm (brachiocephalic), where the vessels are larger and can cope with higher flow, sometimes being preferred to the lower arm (radiocephalic). While there is evidence this approach can reduce non-maturation by as much as 50%, Rotmans claims the higher blood flow in upper arm fistulas creates a fresh set of problems, leading to excessive cardiac output and a greater burden on the heart. “That is one way to circumvent non-maturation but, for me, not the preferred way, because it comes with its own complications in the long term,” he adds.
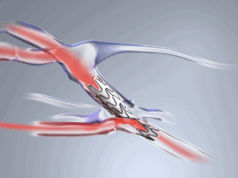
However, another more novel method for influencing haemodynamics in AVFs may be on the horizon, Rotmans says—one that he describes as a “dream solution” in non-maturation. “Ideally, we would have a fistula or vascular access in place that is only functioning during dialysis,” he states. “That would be my ultimate goal.” The phenomenon Rotmans refers to here has been dubbed a ‘dynamic fistula’, whereby a remotely operated valve inside the device can substantially reduce the flow rate through the anastomosis in between dialysis treatments. He notes that the device is currently on the path towards preclinical studies, with data on its safety and efficacy in animal models expected in 2022, but that it may be three or four years before it is ready for widescale clinical trials.
Novel technologies and future research
There is no shortage of further, alternative solutions to non-maturation that are being researched presently. The FA-1 (Fist Assist Devices) and Amplifi (Artio Medical) systems, which are designed to promote vein dilation prior to surgery and boost AVF maturation rates, are interesting recent introductions in this space, according to Rotmans—with the former recently gaining US Food and Drug Administration (FDA) approval and the latter currently in first-in-human studies. Meanwhile, Rotmans describes the growing body of evidence on drug-eluting balloons for dysfunctional AVFs as “promising”, but adds that more studies are required to unravel why there are disparities between the findings of different trials in this space.
Other areas that Rotmans believes warrant further research range from the use of postoperative ultrasound to predict non-maturation—and the benefits of subsequently intervening at an earlier point in time—to the use of artificial intelligence (AI) as a tool for predicting AVF flow profiles, which he adds is an area of “great interest”. “In general, I think we should focus on the haemodynamics in fistulas, and look at a combined therapeutic approach that interferes with multiple pathways at multiple timepoints—we should stop thinking about one solution for the whole problem,” he concludes. “But, it will not be easy to identify optimal timings, dosages and combinations. That will be enough work to occupy everyone involved for the next couple of decades.”