 With 40 years of experience working in nephrology, a passion for advancing the fields of nephrology and kidney disease, and a love of crafting, vascular access marketing manager at Transonic Systems, Deborah Brouwer-Maier (Lansdale, USA), speaks to Renal Interventions about her career as a dialysis nurse, the importance of training and multidisciplinary teams, and her hopes for the future of dialysis care.
With 40 years of experience working in nephrology, a passion for advancing the fields of nephrology and kidney disease, and a love of crafting, vascular access marketing manager at Transonic Systems, Deborah Brouwer-Maier (Lansdale, USA), speaks to Renal Interventions about her career as a dialysis nurse, the importance of training and multidisciplinary teams, and her hopes for the future of dialysis care.
What drew you to your career in haemodialysis vascular access?
I graduated from nursing school and was offered my first job at the same hospital if I would agree to work on the metabolic/renal inpatient ward. At that time, any patient initiated on peritoneal dialysis (PD) or haemodialysis (HD) was admitted to our ward for their first full week of dialysis. We supported their initial education on diet, medications, vascular access or PD catheter care, and the dialysis modality. I quickly became an expert in both continuous ambulatory peritoneal dialysis (CAPD) and cycler dialysis (glass bottles at the time). I was very interested in learning HD as I only observed acute bedside treatments. The dialysis program at the hospital was sold to a dialysis provider, and anyone could apply for a new position, including in their outpatient dialysis centres. I got hired for a new outpatient dialysis centre that was opening much closer to my home. I gained HD experience and then joined a large hospital-based nephrology programme that included all aspects of kidney care, including acute dialysis and transplantation programmes.
My interest in vascular access started when I learned to cannulate arteriovenous (AV) accesses. The training consisted of a see-one-do-one training method. I struggled to find references to support my learning of vascular access and cannulation techniques, so I made it my mission to create a proper training programme to support the theory and practical applications of vascular access cannulation. When I joined the hospital-based programme, I gained more resources to create a proper cannulation training process for new staff. I documented the theory in a publication and created a hands-on cannulation camp training model. The cannulation focus then spread to the general vascular access process for care due to the high incidence of access complications.
Who were your mentors?
From the late 1980s to the early 1990s, vascular access care was very limited. Complications were mainly treated surgically as endovascular interventions had not yet progressed to dialysis access. Clinical trials and other research on vascular access care were minimal. Thus, mentors became the main source of new knowledge to help me increase my knowledge base and impact changes in the process of care related to all aspects of vascular access. I first encountered Susan Boothe as she was the clinical specialist who was supporting polytetrafluoroethylene (PTFE) grafts for haemodialysis. She connected me with Mitchell Henry, and he visited my hospital to help us gain a better understanding of AV access complications and possible treatments. This led to Henry inviting me to be the first nurse to present the nursing perspective of vascular access at the 1995 Symposium on Dialysis Access IV sponsored by the division of transplantation at The Ohio State University, and the book chapter publication. That was the same year as my first publication, entitled Cannulation Camp: Basic Needle Training for Dialysis Staff. My early publications and presentations on cannulation led to my selection to the first Dialysis Outcomes Quality Initiative (DOQI) Vascular Access Guidelines work group. I was honoured to serve with Gerald Beathard, Jack Work, and Anatole Besarab. I am so grateful for their mentorship over the many years they have helped me understand the complex vascular access issues. I went to serve on the Kidney Disease Outcomes Quality Initiative (KDOQI) 2000 and 2006 work groups, thanks to their support.
The names of the many other devoted professionals who have mentored me are too long to list. I strive to pay it forward with my volunteer work with Vascular Access Society of the Americas (VASA), American Society of Diagnostic and Interventional Nephrology (ASDIN), and American Nephrology Nurses Association (ANNA). My mentors taught me that knowledge shared has the most significant impact on a larger number of patients and that the goal is to improve the care of process for all patients requiring dialysis.
Lesley C Dinwiddie was the reviewer for my Cannulation Camp publication. She then became my mentor as she was the trailblazer for the role of vascular access coordinator. Patt Peterson Ryder worked for the arteriovenous fistula (AVF) needle manufactory, and she helped mentor me for cannulation-related topics and assisted me with the Cannulation Camp hands-on programmes. Janet Holland worked with a large dialysis organisation as a vascular access educator and became a key mentor for me. We worked together on many projects, such as the fistula-first initiative, and professional organisations, such as ASDIN and VASA, until her passing last year.
I am incredibly grateful for the many individuals with kidney disease whose care I have had the privilege of being a a part of or have learned from in my many volunteer activities. My most important role has been, and will always be, to serve as an advocate for individuals with kidney disease.
 What, in your view, is the biggest roadblock to further developments in dialysis?
What, in your view, is the biggest roadblock to further developments in dialysis?
In the USA, the business model focuses on the cost/reimbursement of care and profits for the large dialysis providers. For example, the utilisation of point-of-care ultrasound (POCUS) to support improved cannulation is very limited, due to the added cost of the equipment, staff time for the tasks, and lack of separate reimbursement. With the fragmented care system, cost savings for decreased cannulated-related access complications are not savings for the dialysis providers and thus do not offset the additional costs of POCUS.
We need to change the mind-set of cost containment and reimbursement as the driving factors leading to fragmented care, and focus on improved outcomes that can reduce overall costs. For example, the implementation of the end stage kidney disease (ESKD) life plan and access plans is blocked by the fragmented process of care in the USA. The utilisation would help focus care on the patient’s lifespan and, more importantly, meet the patient’s goals for their journey with kidney diseases. This would lead to more innovation, such as innovations in dialysis procedures to allow more patient involvement and self-care. Solutions can be simplified dialysis equipment, devices to assist with single-handed cannulation, needle securement, or needle removal. We have heard the patient’s voice via the Kidney Health Initiative ‘s (KHI) work that a needleless vascular access would be their goal. Shifting the focus to the patient’s point of view with their input can help us change innovation to meet their needs, instead of focusing on the business side and the healthcare professional’s needs.
How important is a multidisciplinary team for the care of dialysis patients?
It is the most critical element. All members of the team are needed to support the best overall care. The need starts with CKD diagnosis and continues as the individual progresses into the later stages of CKD, modality selection (regardless of the modality), and continues throughout an individual’s lifetime. The care is interdependent on the entire multidisciplinary team and must include the patient at the team’s centre. All members bring their unique knowledge base and experience to work collaboratively to create the optimal care plan and respond to challenges as they arise.
What changes would you like to see in dialysis access care?
In my 40-plus years of nephrology, limited advances in cannulation have occurred, including limited improvements to the needle designs. The only two innovations that have gained wide adoption in the USA are safety needles and buttonhole needles. My mentor, Patt Peterson Ryder, helped drive both needle design changes. The safety needles were the direct result of US government’s Occupational Safety and Health Administration publication of the Occupational Exposure to Bloodborne Pathogens standard in 1991. The adoption of other needle designs such as buttonhole needles and longer or shorter needle lengths than the standard one inch needles, is limited due to cost per needle differences. A cannula is currently in a clinical study required for US Food and Drug Administration (FDA) clearance, and the same cost concern will impact the commercialisation of plastic cannulas.
POCUS also lags in adoption due to the cost of the devices and related staff time for training and utilisation. I would like to see POCUS become widely available for cannulation mapping to reduce the number of missed cannulations and infiltrations commonly occurring and accepted as just part of the cannulation process when the complications can be avoided with proper implementation of POCUS.
I would also like to see the full implementation of the ESKD life plan and access plans. As a kidney community, we need to improve the education materials and processes for patients in the earlier stages of CKD. No one can make major life choices like a modality choice, including conservative care or kidney transplantation, without proper educational materials geared toward their current level of knowledge and ones that address the emotional and physical aspects. We need to partner with patients to help
create meaningful educational programs for various stages of CKD. We need to urgently engage patients as new therapies gain adoption to help slow the progression of kidney disease.
How would you expand training for those looking to start a career in haemodialysis vascular access?
We need a standardised cannulation training model based on best practices. The model must include theory and skills training prior to actual patient care. We need an easy-to-use, cost-effective cannulation training device. A new dialysis care professional should not be learning cannulation on an actual patient. We need a simulator for skills training and assessment to ensure the basic cannulation technique is mastered before a needle is inserted into a patient’s vascular access. The patients should not be the test arms for staff learning.
What are your interests outside of medicine?
I love to cook using produce from our garden and from the local farmer’s markets. My son gave me a cookbook as a gift, and we connected via FaceTime to cook recipes together, as he lives too far away to see each other frequently. I enjoy making homemade pasta and sauces.
I also enjoy crafting. I was honoured when my stepdaughter got married, as she allowed me to help design and make the centrepieces as my contribution towards their wedding day.
My gardening time includes both large outside gardens and miniature inside fairy gardens. I design them as gifts to reflect the recipient’s interests.
Homemade gifts are a regular part of my gift-giving as I enjoy making unique things for family and friends.
Fact File
Current appointment:
Vascular access marketing manager, Transonic Systems Inc., Ithaca, USA
Education:
1983: Western Pennsylvania Hospital School of Nursing, Pittsburgh, USA
Honours (selected):
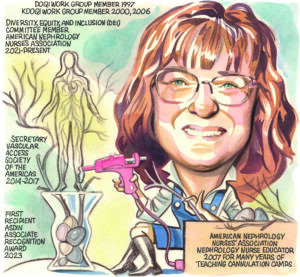
1997: National Kidney Foundation – Special Recognition Award for NKF-DOQI Guideline Work Group Member 1997, and KDOQI 2000, 2006 Work Group Member
2006: Centers for Medicare & Medicaid Service- Certificate of Award for Leadership with the Fistula First Initiative
2007: Centers for Medicare & Medicaid Service Office of Clinical Standards and Quality, Office Director’s Citation for co-chair of the Practitioner Education & Training subcommittee Fistula First
2007: American Nephrology Nurses Association (ANNA) Nephrology Nurse Educator Award
2010: National Kidney Foundation serving the Alleghenies Gift of Life Samll Hands, Big Heart Award
2023: First recipient of the American Society of Diagnostic and Interventional Nephrology (ASDIN) Associate Recognition Award










