 Douglas J Anderson and Jayme E Locke (both Marnix E Heersink School of Medicine, Birmingham, USA) write about genetically edited pig kidney xenotransplantation, the promising results that have been seen from previous studies, and their hopes for the future of this new treatment option for end-stage kidney disease (ESKD).
Douglas J Anderson and Jayme E Locke (both Marnix E Heersink School of Medicine, Birmingham, USA) write about genetically edited pig kidney xenotransplantation, the promising results that have been seen from previous studies, and their hopes for the future of this new treatment option for end-stage kidney disease (ESKD).
Kidney transplantation remains the best available treatment for ESKD. Sadly, most patients will not realise the benefits of kidney transplant due to the shortage of donor organs; many patients die waiting for a transplant and many more are never listed. Xenotransplantation, using an animal as the donor, offers the opportunity to end this shortage.
Decades of effort placed into exploring the immunobiology of cross-species transplantation yielded increased understanding of the barriers to xenotransplantation. Pigs emerged as the preferred donor due to rapid growth, early and frequent reproduction with large litters, and relative ease of husbandry.1 However, preformed antibodies lead to rapid hyper-acute rejection of untreated pig xenografts. Genetic modification of the donor animal offered a solution to this issue, and furthermore allows for introduction of human regulatory genes to further ameliorate the human anti-pig response. However, introducing multiple genetic modifications into a large mammal remained a significant challenge until the advent of CRISPR-Cas9 technology. Now, we have produced donor animals with up to 69 genetic edits.2
The genetic modifications of the donor pig both reduce the burden of preformed antibodies, but also make the pig xenograft more “human-like” in the view of the recipient immune system. Various genetic modifications have been introduced. Virtually all constructs utilise knockout of the Gal antigen, which accounts for the majority of preformed antibodies. Other modifications that have been employed include knockout of two other carbohydrate xenoantigens and introduction of a variety of human transgenes: thrombomodulin, endothelial cell protein C receptor, CD47, haem oxygenase-1 (HO-1), CD46, decay accelerating factor, and a human tumour necrosis factor regulator.2,3 Genetic manipulation can also address practical concerns, such as knockout of the growth hormone receptor to reduce post-transplant organ growth or deletion of all copies of the porcine endogenous retrovirus (PERV) genome as a safety measure.2,4 What combination of genetic edits is optimal, and which could alternatively be managed pharmacologically, or by careful husbandry and screening in the case of the PERV genome, remains to be seen.
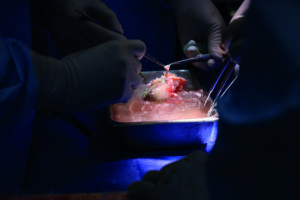
Preclinical work using genetically modified pig kidneys has yielded promising results. Xenokidneys have provided life-sustaining renal function in non-human primates for over two years.2 In the Parsons model, using a brain-dead human recipient, renal function with clearance of creatinine and maintenance of physiologic homeostasis has been demonstrated, and this can be accomplished with standard, clinically available immunosuppression.3,5,6 While hyper-acute rejection is relatively easily avoided at this point, thorough investigation of the human immune response to the pig xenograft has yielded mixed results, likely owing to differences in the exact genetic construct used and differing immunosuppressive protocols.7,8 Transmission of PERVs and other porcine viruses, such as porcine cytomegalovirus (CMV) can be avoided with careful screening of the donor herd.3 Two living patients have now been the recipients of porcine kidneys, reportedly with initial graft function.9,10
The promising results of these translational studies suggest we have reached the point where xenotransplantation should be studied in a systematic clinical trial to address remaining knowledge gaps. The longevity of a xenotransplant remains a significant unanswered question: is this destination therapy or merely a bridge to allotransplantation? What is the optimal combination of genetic modifications and immunosuppressive protocols? Will zoonotic infection remain a concern over longer periods of time? These are all questions that will need to be addressed in a systematic way, and in larger numbers than individual case reports or even small series. The time for a clinical trial is now, in hopes that we can end the organ shortage.
Collaboration between medical teams, engineers and patients is crucial for advancing such technologies in haemodialysis access. Collaboration with patients and caregivers, meanwhile, is equally vital, and involving them in the design and testing process ensures that the solutions developed truly meet the needs and preferences of those who will use them. Patient feedback is invaluable when refining wearable devices and algorithms so that they are user-friendly, reliable, and well-integrated into patients’ daily lives.
Disclosures: Anderson and Locke have received research support/grants from United Therapeutics and its subsidiaries, Revivicor and Lung Biotechnologies.
References:
- Sachs DH. The pig as a potential xenograft donor. Vet Immunol Immunopathol. 1994 Oct;43(1–3):185–91.
- Anand RP, Layer JV, Heja D, et al. Design and testing of a humanized porcine donor for xenotransplantation. Nature. 2023 Oct 12;622(7982):393–401.
- Porrett PM, Orandi BJ, Kumar V, et al. First clinical-grade porcine kidney xenotransplant using a human decedent model. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2022 Apr;22(4):1037–53.
- Hansen-Estruch C, Iwase H, Jagdale A, et al. Initial Experience with Growth Hormone Receptor Knockout in Pig-to-Baboon Kidney Transplantation: Effect on Ureteric Viability and Kidney Growth [abstract]. Am J Transplant [Internet]. 2021. Available from: https://atcmeetingabstracts.com/abstract/initial-experience-with-growth-hormone-receptor-knockout-in-pig-to-baboon-kidney-transplantation-effect-on-ureteric-viability-and-kidney-growth/
- Locke JE, Kumar V, Anderson D, et al. Normal Graft Function After Pig-to-Human Kidney Xenotransplant. JAMA Surg. 2023 Oct 1;158(10):1106.
- Jones-Carr ME, Fatima H, Kumar V, et al. C5 inhibition with eculizumab prevents thrombotic microangiopathy in a case series of pig-to-human kidney xenotransplantation. J Clin Invest. 2024 Jan 25;134(5):e175996.
- Loupy A, Goutaudier V, Giarraputo A, et al. Immune response after pig-to-human kidney xenotransplantation: a multimodal phenotyping study. The Lancet. 2023 Sep;402(10408):1158–69.
- Cheung MD. Spatiotemporal immune atlas of a clinical-grade gene-edited pig-to-human kidney xenotransplant. Nat Commun. 2024;15:3140.
- Chase B. World’s First Genetically-Edited Pig Kidney Transplant into Living Recipient Performed at Massachusetts General Hospital [Internet]. 2024. Available from: https://www.massgeneral.org/news/press-release/worlds-first-genetically-edited-pig-kidney-transplant-into-living-recipient
- DeVries C. First-Ever Combined Heart Pump & Gene-Edited Pig Kidney Transplant Gives New Hope to Patient with Terminal Illness [Internet]. 2024 [cited 2024 Apr 25]. Available from: https://nyulangone.org/news/first-ever-combined-heart-pump-gene-edited-pig-kidney-transplant-gives-new-hope-patient-terminal-illness











