Autogenous fistulas offer advantages to haemodialysis patients, long-term survival and low rates of complication among them. But failed or slow maturation as well as the risk of early thrombosis frequently “offset” these advantages and result in the use instead of a central venous catheter. Such “serious limitations”, write the authors of a new study published in the Journal of Vascular Access (JVA), demand the evaluation of alternative options.
Autogenous fistulas offer advantages to haemodialysis patients, long-term survival and low rates of complication among them. But failed or slow maturation as well as the risk of early thrombosis frequently “offset” these advantages and result in the use instead of a central venous catheter. Such “serious limitations”, write the authors of a new study published in the Journal of Vascular Access (JVA), demand the evaluation of alternative options.
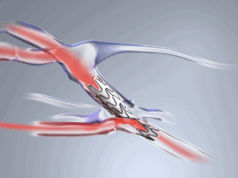
Among those are biological regenerative conduits. Lead author Adrian Ebner (Sanatorio Italiano, Asuncion, Paraguay), alongside fellow researchers including Haimanot Wasse (RUSH Medical College, Chicago, USA) and corresponding author Zeeshan Syedain (University of Minnesota, Twin Cities, USA), focused on the TRUE AVC (Vascudyne) tissue-engineered vascular conduit and aimed to establish whether it could demonstrate “functional patency, lack of infection, and a low adverse event rate”.
Ebner et al’s new study is the first to examine a novel tissue-engineered vascular conduit “cultured from completely biologic raw materials and allogeneic dermal cells”, which had previously been trialled in non-human primate models. That study found no immune response, while “dialysis needle puncture sites demonstrated normal healing with no reduction in mechanical strength of the conduit”. The study provides an alternative to the work of Jeffrey H Lawson (Duke University, Durham, USA) and colleagues in a Lancet-published investigation from 2016, which found that a bioengineered human acellular vessel “seem[ed] to provide safe and functional haemodialysis access”, promising a step up from polytetrafluoroethylene arteriovenous grafts and their associated thrombosis and infection risks.
Following from this, Ebner and colleagues designed their first-in-human study to look at the outcomes from five patients who received an implant of the conduit “in an initial evaluation of [its] clinical safety and performance”. Patients were selected as long as they were aged 18–75, were diagnosed with end-stage kidney disease (ESKD)—with one exception who was pre-ESKD—and were either on dialysis or intended to initiate it within 12 weeks.
They explain the process behind the conduit’s development: “In brief, allogeneic human dermal fibroblasts are seeded in fibrin gel and cultured in a bioreactor to create a tubular conduit. Cellular material is then removed to create an off-the-shelf extracellular matrix which can be repopulated with host cells.” The TRUE AVC conduit “was tested in vitro to ensure final product is suitable for implant”.
Primary efficacy endpoints of the study were primary patency, assisted primary patency, and secondary patency at 26 weeks, plus successful dialysis through to six months. Ultrasound and physical examination were used for assessment. Among the secondary endpoints was immune system response to the implant, while primary safety endpoints included freedom from clinically significant aneurysm and anastomotic bleeding.
The authors state that the conduit “handled well surgically, with properties similar to that of the native human vein”. Conduit flow following the procedure was “excellent in all cases,” meanwhile, “averaging 1098±388ml/min at week four and remaining stable through 1248±355ml/min at 26 weeks”. There was no significant change in surgical site healing compared to regular conduits, with no oedema or erythema found at four weeks. Primary patency at six months was found to be 80%, with secondary patency recorded at 100%. There was no infection in any of the patients, all of whom received dialysis, nor was there statistically significant change in the diameter of the conduit on ultrasound examination. The authors also note that “no specific IgG antibody response was seen in any patients”, and add that one patient required reintervention for thrombus removal at five months.
Highlighting the similarity of the conduit’s handling characteristics to a native vein, its successful provision of dialysis, and its lack of infection or immune response, Ebner and colleagues say the results demonstrate “the initial and early safety of TRUE AVC”. They turn in their discussion to the Kidney Disease Outcomes Quality Initiative (KDOQI) 2019 guidelines, which call for “reliable, complication-free access” for dialysis. While arteriovenous fistulas (AVFs) are generally preferred to arteriovenous grafts (AVGs), they argue, AVFs’ potential for maturation failure or delay “should be considered” nonetheless.
The authors state: “An off-the-shelf, completely biological acellular vascular conduit, able to repopulate with the recipient’s own cells and become a living vessel in vivo, may provide long-term functional patency and low complication rates similar to the native fistula, while avoiding maturation failures and early thrombosis.”
Speaking exclusively to Renal Interventions, Syedain also said: “Completely biological regenerative tissue conduits are designed to mimic the structure and function of natural blood vessels, potentially improving longevity and performance of haemodialysis graft. This study demonstrate initial safety, mechanical durability and lack of immune response with TRUE AVC and as a potential off-the-shelf blood vessel conduit for clinical use.”
Looking forward, Ebner et al point out that larger cohort studies are planned to further investigate the safety and efficacy of TRUE AVC.