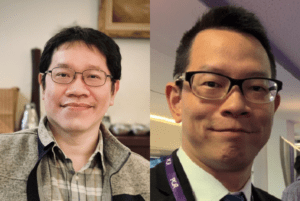
 Recent studies have evaluated drug-coated balloon (DCB) treatments’ ability to help maintain arteriovenous fistula (AVF) patency for haemodialysis patients “with mixed results”, according to Mu-Yang Hsieh (National Yang Ming Chiao Tung University, Hsinchu, Taiwan). However, he and co-authors including corresponding author Chih-Cheng Wu (National Taiwan University Hospital Hsin-Chu Branch, Hsinchu, Taiwan) contend that these studies have excluded stenoses that involve stent grafts—a subject to which they have now turned their attention in a new randomised controlled trial (RCT).
Recent studies have evaluated drug-coated balloon (DCB) treatments’ ability to help maintain arteriovenous fistula (AVF) patency for haemodialysis patients “with mixed results”, according to Mu-Yang Hsieh (National Yang Ming Chiao Tung University, Hsinchu, Taiwan). However, he and co-authors including corresponding author Chih-Cheng Wu (National Taiwan University Hospital Hsin-Chu Branch, Hsinchu, Taiwan) contend that these studies have excluded stenoses that involve stent grafts—a subject to which they have now turned their attention in a new randomised controlled trial (RCT).
Their research is published in the European Journal of Vascular and Endovascular Surgery and compares the advantages of DCB treatment with those of conventional angioplasty in patients with stent grafts. The authors contend that intimal hyperplasia recurs at the edges of stent grafts in many of those patients who receive one, something which they note may be limited by paclitaxel, “the most commonly used drug in DCBs”.
With that in mind, the authors designed a single-centre, prospective, randomised controlled trial enrolling 40 patients with stent grafts, half of whom were assigned to a paclitaxel DCB arm and half of whom received plain balloon angioplasty. The authors note that the primary inclusion criterion was stent graft implantation in a patient with dysfunctional AVF or AV graft (AVG), with dysfunction designated as their having at least one clinical indicator as defined by the Kidney Disease Outcomes Quality Initiative (KDOQI) guideline.
The authors further detail that study patients underwent fistulography in order to assess whether they had stent graft stenosis >50% within the access circuit, while they state that the DCB chosen was an angioplasty balloon with a 2μg/mm2 paclitaxel-based coating, 135cm shaft length, 4–8mm diameter, and 40–100mm length.
Describing the procedure, they note that in the DCB group the target lesion was dilated to nominal pressure for 120 seconds, before the DCB was inflated to a nominal pressure, with the diameter “required to equal that of the initial dilatation balloons”. In the control group, angioplasty with a pre-dilatation balloon was performed again for 120 seconds.
Citing the “greater statistical power for a continuous endpoint” in a small RCT, Hsieh et al chose late luminal loss of the target lesion as their primary endpoint, and they evaluated minimal luminal diameter (MLD) at zero and six months using angiography. Secondary endpoints included target lesion primary patency and access circuit primary patency at six months, with the former defined as “no clinically driven reintervention on the target lesion” while access circuit patency “ended with any intervention on the access circuit”.
In total, angiographic follow-up was performed in 18 patients from each group. The late loss of MLD in the DCB group was found to be 1.82±1.83mm, which the authors describe as “significantly lower” than the mean late loss of 3.63±1.08mm in the control group (p=0.001). The 6-month target lesion primary patency interval for the DCB group was 159±49 days and 93±67 days for the conventional angioplasty group (p=0.008). Hsieh et al state that these results “demonstrated that drug-coated balloons prevented late luminal loss of stent-graft stenosis and potential superior primary target lesion patency over conventional balloons”.
“With the increasing use of stent-grafts, stenosis of the stent graft edge will become a common problem,” they add, making reference to the results of the RENOVA study. It is with this problem that they contextualise their own finding that “the absolute risk difference between the two groups [in our trial] was larger than that observed in DCB trials for AVFs”. They also make the conclusion that the edge of a stent graft is a location of particular risk for restenosis given their data—something they suggest has not been addressed previously.
Turning to the limitations of their study, they describe it as “substantially underpowered for binary outcomes”, and they call for a “much larger trial” to validate their results. They also say that the trial was too small to designate clinical endpoints. Nevertheless, they conclude that convention angioplasty is not a “durable” solution to stent graft stenosis. DCBs, they say, offer a potential solution to the problem of patency.












